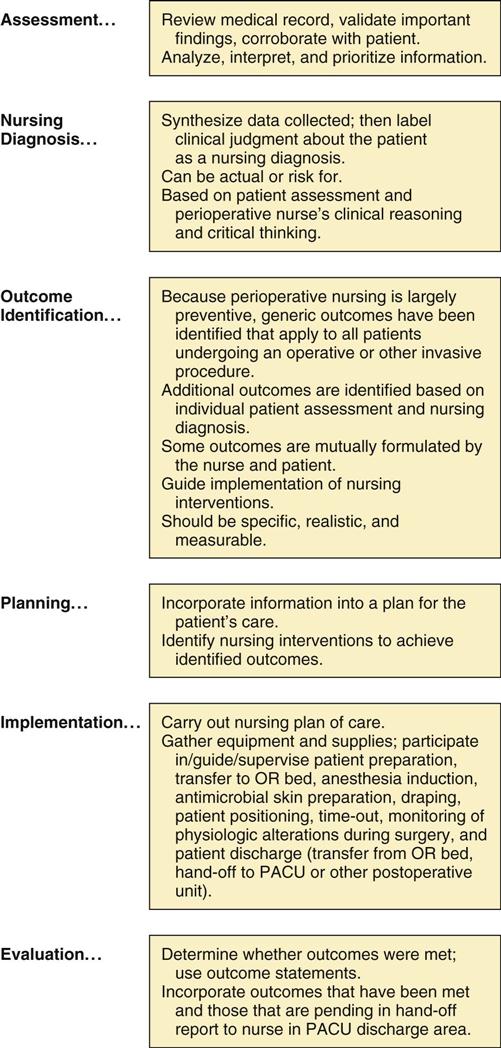
Victoria M. Steelman Perioperative nursing is the nursing care provided to patients before, during, and after surgical and invasive procedures. Nurses practice this specialty in surgical suites, ambulatory surgery centers, endoscopy suites, laser centers, interventional radiology departments, mobile surgical units, and physicians’ offices across the United States and the world. Perioperative nursing includes a broad array of cutting-edge innovations, such as remote surgery, virtual endoscopy, robotics, computerized navigation systems for neurosurgery, transplanted tissue and organs, biologic materials that are absorbed to replace worn-out body parts, radiofrequency identification (RFID), transoral approaches (natural orifice surgery), and electronic health records (EHRs). In this high-tech era, perioperative patient care is very different than it was in the past. In the past, the term operating room (OR) nursing was used to describe the care of patients in the immediate preoperative, intraoperative, and postoperative phases of the surgical experience (Figure 1-1). This term implied that nursing care activities were limited to the physical confines of the surgical suite. The term may have contributed to stereotypic images of the OR nurse who took care of the OR and its equipment, but who had little if any interaction or nursing responsibility for medicated and anesthetized patients in the surgical suite. With such an image, nurses practicing outside the OR had difficulty crediting important elements of the nursing process and patient care accountability to the nurse who practiced “behind the double doors” of the surgical suite. Today, perioperative nursing implies the delivery of comprehensive patient care within the preoperative, intraoperative, and postoperative periods of the patient’s experience during operative and other invasive procedures, using the framework of the nursing process. In doing so, the perioperative nurse assesses the patient—collects, organizes, and prioritizes patient data; establishes nursing diagnoses; identifies desired patient outcomes; develops and implements a plan of nursing care; and evaluates that care in terms of outcomes achieved by and for the patient. Throughout, the perioperative nurse functions both independently and interdependently. As with nurses in other specialties, the perioperative nurse collaborates with other healthcare professionals, makes appropriate nursing referrals, and delegates and supervises other personnel in providing safe and efficient patient care. When nurses practice perioperative nursing in its broadest sense, care may begin in the patient’s home, a clinic, a physician’s office, the patient care unit, the presurgical care unit, or the holding area. After the surgical or invasive procedure, care may continue in the postanesthesia care unit (PACU) and evaluation of patient outcomes may extend onto the patient care unit, in the physician’s office, in the patient’s home, in a clinic, or through written or telephone patient surveys. When nurses practice perioperative nursing in its more limited sense, patient care activities may be confined to the common areas of the surgical suite. Assessment and data collection may take place in the holding area, whereas evaluation may take place on discharge from the OR. Regardless of the way nurses practice perioperative nursing in a healthcare setting, it remains based on the nursing process and professional nursing practice. The perioperative nurse also functions as a patient advocate during times of vulnerability. This specialty requires a broad knowledge base, instant recall of nursing science, an intuitive ability to be guided by nursing experience, and diversity of thought and action, as well as great stamina and flexibility. Whether a generalist or a specialist, the perioperative nurse depends on knowledge of surgical anatomy, physiologic alterations and their consequences for the patient, intraoperative risk factors, potentials for and prevention of patient injury, and psychosocial implications of surgery for the patient and family. This knowledge enables the perioperative nurse to anticipate needs of the patient and surgical team and to rapidly initiate safe and appropriate nursing interventions. This too is part of patient advocacy—that is, doing for the patient what needs to be done to provide a safe and caring environment. The Association of periOperative Registered Nurses (AORN) has asserted the significance of such safety by reaffirming that staffing of healthcare personnel must ensure that patients undergoing surgical and invasive procedures have a perioperative nurse as circulator in the OR, and also that the core activities of perioperative nursing care (assessment, diagnosis, outcome identification, planning, and evaluation) be completed by a perioperative nurse (AORN, 2012a). A significant part of perioperative nursing is the delivery of scientifically based care. Such care implies understanding the rationale for certain activities and interventions, knowledge of how and when to implement them, and the skills to evaluate safety, cost-effectiveness, and outcomes of the care delivered. This knowledge empowers the perioperative nurse to anticipate and prepare for the next steps of the surgical procedure and understand their concomitant implications for the patient and for the surgical team. Scientific nursing interventions, critical thinking and clinical reasoning, and caring, comforting behaviors are at the heart of perioperative nursing. Unit II focuses on surgical procedures common to inpatient and ambulatory settings. Each chapter in Unit II contains a Sample Plan of Care with suggested nursing interventions. A fundamental assumption throughout this textbook is that perioperative nursing is a blend of technical and behavioral care and that critical thinking is the underpinning for caring for patients professionally. Good clinical judgment derives from critical thinking (Sullivan, 2012). Critical thinking requires purposeful, outcomes-directed thought and is driven by patient need. It is based on the nursing process and nursing science. Further, critical thinking requires knowledge, skills, and experience guided by professional standards and ethics and grounded in constant reevaluation, self-correction, and continual striving to improve. AORN has developed a model to describe the important relationship between the patient and the perioperative nursing care provided. The Perioperative Patient Focused Model (AORN, 2012b) consists of domains or areas of nursing concern: nursing diagnoses, nursing interventions, and patient outcomes. These domains are in continuous interaction with the health system that encircles the focus of perioperative nursing practice—the patient (AORN, 2011a). Three of these domains—behavioral responses, patient safety, and physiologic responses—reflect phenomena of concern to perioperative nurses and comprise the nursing diagnoses, interventions, and outcomes that surgical patients or their families experience. The fourth domain, the health system, comprises the structural data elements and focuses on clinical processes and outcomes. The model illustrates the dynamic nature of the perioperative patient experience and the nursing presence throughout that process. Working in a collaborative relationship with other members of the healthcare team and the patient, the nurse establishes outcomes, identifies nursing diagnoses, and provides nursing care. The nurse intervenes within the context of the healthcare system to help the patient achieve the highest attainable health outcomes (physiologic, behavioral, and safety) throughout the perioperative experience. The Perioperative Patient Focused Model (AORN, 2011b) emphasizes the outcomes-driven nature of perioperative patient care. Perioperative nurses possess a unique understanding of desired outcomes that apply to all patients. In contrast to some nursing specialties in which nursing diagnoses are derived from signs and symptoms of a condition, much of perioperative nursing care is preventive in nature, based on knowledge of risks inherent to patients undergoing surgical and invasive procedures. Perioperative nurses identify these risks and potential problems in advance, and direct nursing interventions toward prevention of undesirable outcomes, such as injury and infection. Based on an individual patient assessment, the perioperative nurse identifies relevant nursing diagnoses. This information guides the nursing interventions for each patient. From admission through discharge and home follow-up, the perioperative nurse plays a major role in managing the patient’s care. Research based on the Perioperative Patient Focused Model (AORN, 2011b) continues to test and validate the contributions of perioperative nurses to patient outcomes in the variety of settings in which this nursing specialty is practiced. Perioperative nursing is a systematic, planned process—a series of integrated steps. For professional nursing, national standards establish the full expectations of the professional role within which the nurse practices. In the 1960s, the American Nurses Association (ANA) engaged in standards development. First published in 1973, these standards helped to shape nursing practice. Specialty nursing organizations, including AORN, have worked with the ANA to develop their own standards and guidelines using the ANA framework. This collaboration has resulted in the use of common language and a consistent format for the profession. AORN (2013a) has developed a set of standards for perioperative nursing care (Box 1-1). These standards are authoritative statements that define and enumerate the responsibilities for which perioperative nurses are accountable. The standards represent a comprehensive approach to meeting the healthcare needs of surgical patients. AORN’s nursing standards are categorized as either structure or process. AORN (2013a) Standards of Perioperative Administrative Practice are structure standards that describe organizational characteristics, administrative and fiscal accountabilities, personnel qualifications, and facilities and environmental requirements. These standards provide authoritative guidance for professionals in administrative roles and provide the structure within which perioperative patient care should be provided. Process standards relate to nursing activities, interventions, and interactions. They are used to explicate clinical, professional, and quality objectives in perioperative nursing. The three AORN (2013a,b) process standards are the Standards of Perioperative Nursing, Standards of Perioperative Professional Practice, and Quality and Performance Improvement Standards for Perioperative Nursing. Standards of Perioperative Nursing constitute standards of care and professional performance (AORN, 2013a). Standards of care are based on and describe the application of the nursing process in perioperative nursing. They include the collection and analysis of health data, identification of expected outcomes, planning and implementation of patient care, and evaluation of the effects of this care on patient outcomes. AORN (2013a) Standards of Perioperative Professional Practice require, in part, that the perioperative nurse evaluate the effectiveness of nursing practice and the quality of that practice. These professional practice standards also require perioperative nurses to evaluate their own practice. Achieving certification (certified nurse, operating room [CNOR]), pursuing lifelong learning, and maintaining competency and current knowledge in perioperative nursing are hallmarks of the professional. One of the standards focuses on the importance of evidence-based practice (EBP) and participation in the generation of new knowledge through research. The pace and complexity of advances in surgical procedures, minimally invasive surgery, new technologies, professional nursing issues, ongoing healthcare reform measures, continuing changes in recommended practices, and the burgeoning body of nursing research and best practice guidelines demand constant professional education and development. Perioperative professionals must continue to research patient outcomes, to link nursing interventions to outcomes, and to develop methods that conserve resources when implementing interventions. Other standards of professional practice address ethics, collaboration, and collegiality. The third set of process standards, AORN (2013b) Quality and Performance Improvement Standards for Perioperative Nursing, delineate perioperative nurses’ responsibilities to evaluate the patient care provided and to optimize patient outcomes. This set of standards underscores the importance of analyzing and using data to improve patient care. Looking at nursing as a process brings it into perspective as a system of critical thinking that provides the foundation for nursing actions (Figure 1-2). The focus of the nursing process is the patient, and prescribed nursing interventions are those that meet patient needs. Given the setting and the nature of the work, perioperative nursing is particularly susceptible to being seen as only an accumulation of mechanical techniques and the execution of surgeon orders. By using the nursing process, however, perioperative nurses can focus on the patient and, at the same time, use skills and knowledge to care for patients and to make independent judgments and clinical decisions. Use of the nursing process, nursing plans of care, clinical pathways, and best practices (discussed later in this chapter) has become an integral part of patient care. In its simplest form, the nursing process defined by the ANA consists of the following six steps: assessment, nursing diagnosis, outcome identification, planning, implementation, and evaluation. The process is dynamic and continual. Also, in all areas of nursing practice, certain responsibilities are inherent in the nursing process: (1) providing culturally and ethnically sensitive, age-appropriate care; (2) maintaining a safe environment; (3) educating patients and their families; (4) ensuring continuity and coordination of care through discharge planning and referrals; and (5) communicating information. Assessment is the collection and analysis of relevant health data about the patient. Sources of data may be a preoperative interview with the patient and the patient’s family; review of the planned surgical or invasive procedure; review of the patient’s medical record; examination of the results of diagnostic tests; and consultation with the surgeon and anesthesia provider, unit nurses, or other personnel. Data collection focuses on these major elements: (1) the patient’s current diagnosis, physical status, and psychosocial status (including literacy, language skills, and spiritual, ethnic, cultural, and lifestyle information relevant to the delivery of patient-specific care); (2) previous hospitalizations or surgical interventions, and serious illnesses; and (3) the planned surgical or invasive procedure and the patient’s understanding of this plan. Implementing patient-centered care (Patient-Centered Care) requires the perioperative nurse to encourage the patient’s active involvement in his or her care as part of patient safety. Of primary importance are the patient’s and family’s understanding of the scheduled procedure and the patient’s participation in activities such as marking the surgical site (Patient Safety) (the Universal Protocol for correct site surgery, along with other National Patient Safety Goals, is discussed in Chapter 2) (TJC, 2013). The perioperative nurse also assesses risk factors that may contribute to negative outcomes. The perioperative nurse proactively reports any concerns (e.g., abnormal laboratory values, or issues related to the patient’s lack of understanding of the planned procedure) to the surgeon, documents all data collected, and notes any referrals that he or she makes. The assessment format varies from institution to institution but always includes the physiologic and psychosocial aspects of the patient. In some settings the assessment is done in stages by one or more perioperative nurses. A perioperative nurse may perform an assessment in the presurgical care unit or by telephone before the day of surgical admission. In such cases the nurse in the OR verifies parts of the assessment previously done and completes the remainder. For a perioperative nurse caring for a healthy patient, assessment may mean only a thoughtful, brief review of the assessments previously done, a short patient interview, review of the medical record and surgical procedure, and a mental rehearsal of the resources and knowledge necessary to guide the patient successfully through an operative course. At other times, the perioperative nurse assesses all aspects of the patient and the patient’s condition thoroughly, along with preoperative and postoperative reviews. When developing guidelines for preoperative assessment, patient and family education, and discharge planning, the perioperative nurse considers the following: • Is relevant, concise patient information already available to the perioperative nursing staff? • Is sufficient time available to initiate a meaningful perioperative nurse-patient interaction? • Is there continuity of care between the perioperative unit and other nursing care units? Being able to exchange information about patients in face-to-face meetings, by telephone, or by written messages is helpful for unit and perioperative nurses. A thorough assessment made and recorded by the preoperative nurse can accompany patients to the OR and serve as a guide for the perioperative nurse, who then completes a more focused preoperative patient assessment. With the burgeoning number of ambulatory surgery procedures, preoperative assessment is often integrated with preadmission testing. Some institutions hold group preoperative sessions. These not only help nurses get to know the patients, but also permit nurses to impart information on common routines, reactions, sensations, and nursing procedures that will take place preoperatively, intraoperatively, and postoperatively. The perioperative setting determines the type of interaction that may occur. The use of preoperative phone calls and on-line questionnaires has also gained wide acceptance. The important point is that some form of assessment, patient and family education, and discharge planning must be done. The particular facility and nursing staff determine how to accomplish it. Assessment requires that the nurse know and understand the patient as a feeling, thinking, and responsible individual who is a candidate for a surgical or invasive procedure. Data identified through assessment help the perioperative nurse meet unique patient needs throughout the surgical intervention. Based on the data collected, recorded, and interpreted during patient assessment, the perioperative nurse then formulates a nursing diagnosis. Nursing diagnosis is the process of identifying and classifying data collected in the assessment in a way that provides a focus to plan nursing care. Nursing diagnoses have evolved since they were first introduced in the 1950s. Today they are identified, named, and classified according to human response patterns and functional health patterns. The authoritative organization responsible for delineating the accepted list of nursing diagnoses is the North American Nursing Diagnosis Association International (NANDA-I) (Box 1-2). Each NANDA-I–approved nursing diagnosis has a set of components, as follows: a definition of the diagnostic term; its defining characteristics (i.e., the requisite pattern of signs and symptoms or cues that make the meaning of the diagnosis clear); and its related or risk factors (i.e., causative or contributing factors that are useful in determining whether the diagnosis applies to a particular patient). For perioperative patients, many nursing diagnoses are “risk” diagnoses, meaning that they are not evidenced by signs or symptoms because the problem has yet to occur and nursing interventions are directed at prevention. Not all patient problems encountered in the perioperative setting can be described by the list of accepted NANDA-I nursing diagnoses. Perioperative nurses must participate in describing and naming new nursing diagnoses that characterize unique perioperative patient problems. NANDA-I has established a “to be developed” category to designate nursing diagnoses that are partially developed and deemed useful to the nursing profession; perioperative nurses may develop unique diagnostic labels and definitions, and work to develop and validate them further through this process. This constructive process becomes even more important as healthcare moves toward the use of information systems to document nursing practice. Outcome identification describes the desired or favorable patient condition that can be achieved through nursing interventions (Box 1-3). The study of patient outcomes is not new. To be useful for assessing the effectiveness of nursing care, patient outcomes should be “nursing-sensitive”; they should be influenced by nursing and describe a patient state that can be measured and quantified. Nursing-sensitive patient outcomes derive from nursing diagnoses and direct the interventions that resolve the nursing diagnoses. They are the standards or criteria by which the effectiveness of interventions is measured. Outcomes are stated in terms of expected or desired patient behavior and must be specific and measurable. The appropriate time to measure perioperative nursing-sensitive outcomes varies.
Concepts Basic to Perioperative Nursing
Overview of Perioperative Nursing Practice
Perioperative Patient Focused Model
Standards of Perioperative Nursing Practice
Perioperative Nursing Practice Standards
Nursing Process
Assessment.
Nursing Diagnosis.
Outcome Identification.
Basicmedical Key
Fastest Basicmedical Insight Engine