Collis Gastroplasty
John G. Hunter
Mark J. Eichler
DEFINITION
Encountering a foreshortened esophagus during surgery at the hiatus, a lengthening procedure is necessary for adequate distal abdominal esophageal length for an antireflux procedure. First described in Thorax by John Leigh Collis in 1957 for patients with a short esophagus and hiatal hernia, with or without reflux, a gastroplasty is performed via a thoracotomy on the left aspect of the herniated proximal stomach.1 This technique has subsequently evolved through thoracoscopic and laparoscopic means for hiatal hernia repairs as well as reflux disease in order to lengthen the abdominal portion of the esophagus for an adequate axial distance around which to perform gastric fundoplication. The Collis gastroplasty commonly involves a laparoscopic stapling technique about the gastroesophageal junction (GEJ) by removing a wedge of stomach at the angle of His, thereby lengthening the effective distal esophageal dimension intraabdominally, about which a fundoplication can be wrapped.2
PATIENT HISTORY AND PHYSICAL FINDINGS
Secondary to chronic acid inflammation and subsequent fibrotic remodeling of the distal esophagus, approximately 10% to 25% of patients with reflux have a shortened esophagus.3,4 The majority of these patients, however, do not need an esophageal lengthening procedure for a tension-free fundoplication if adequate mediastinal dissection gains return of abdominal esophageal length.5 Sufficient intraabdominal length can be evidenced by the GEJ lying intraabdominally with a distance between the diaphragmatic hiatus and the GEJ of at least 2.5 cm. It is at this threshold of 2.5 cm (approximately the length of a fully opened atraumatic laparoscopic grasper) after adequate mediastinal and crural dissection should the decision to perform a Collis gastroplasty take place,3 with an overall incidence of implementation of 3% to 4% of reflux operations.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The preoperative workup for reflux disease spans endoscopy (esophagogastroduodenoscopy [EGD]), esophagography (upper gastrointestinal contrast swallow or esophagram), manometry, and pH probe testing. However, there is no gold-standard radiologic imaging study for preoperative preparation in reflux disease, as the surgical decision making to perform a Collis gastroplasty is done ultimately intraoperatively. Yet, esophagography and endoscopy may be the optimal studies to demonstrate a foreshortened esophagus by the following signs6:
Hiatal hernia of 5 cm or more
Giant type III paraesophageal hernia (FIG 1)
Esophagitis, Barrett’s changes, and/or stricture
SURGICAL MANAGEMENT
Preoperative Planning
Because the Collis gastroplasty is an adjunctive procedure during gastric fundoplication, the principles of a proper antireflux procedure (wrap) or gastropexy apply, including left and right crural exposure, adequate mediastinal dissection, atraumatic esophageal retraction, and division of the short gastric vessels. Please refer to Part 1, Chapters 19 and 22 for further details.
All studies, including esophagram, EGD, manometry, and pH testing should be readily available and reviewed prior to and at the time of surgery. The esophagram should be displayed on a spare or dedicated monitor in the operating theater and EGD images be loaded as well for intraoperative reference.
Attention to fine detail of the manometric report may avoid an unnecessary and detrimental 360-degree fundoplication, as a complete wrap may worsen symptoms in the light of the following findings7:
Severe esophageal dysmotility
Very low residual postrelaxation lower esophageal sphincter (LES) pressures less than 30 mmHg during wet swallow
Positioning
Although there are many port placement techniques, the stapled Collis gastroplasty necessitates a left upper quadrant, endoscopic, angulating stapler by the surgeon’s right hand through a 12-mm trocar. Steep reverse Trendelenburg is the position of choice (FIG 2).
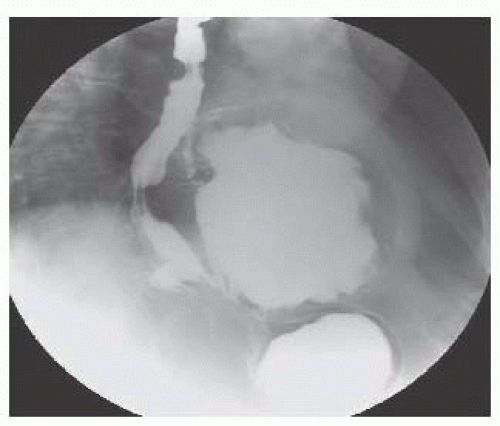
FIG 1 • Esophagram demonstrating tortuous esophagus with shortening, distal narrowing or strictures, and a type III paraesophageal hiatal hernia.
Assume extensive mediastinal dissection will be warranted, and therefore, risk of pleural compromise (FIG 3). The sterile skin preparation must be wide enough on either flank in case tube thoracostomies are necessary from resultant pneumothorax. However, a red rubber catheter between 10 and 14 Fr may be placed in a witnessed pleural defect intraabdominally spanning the diaphragm to the hemithorax in question. This reduces the resultant pneumothorax and peak ventilatory pressures with the aid of lowering insufflation pressures as well as anesthesia-assisted ventilatory Valsalva.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


