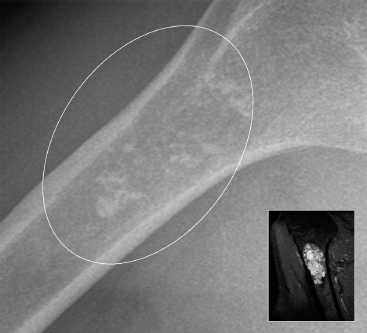
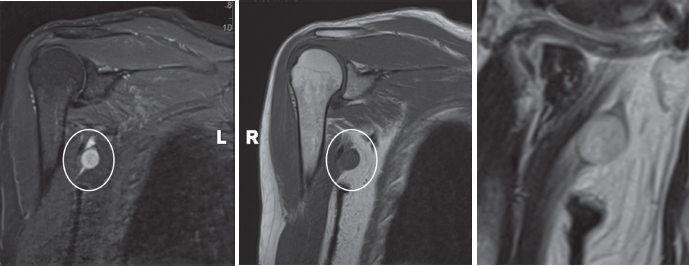
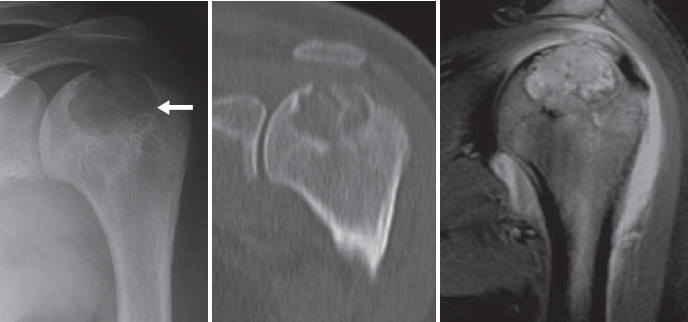
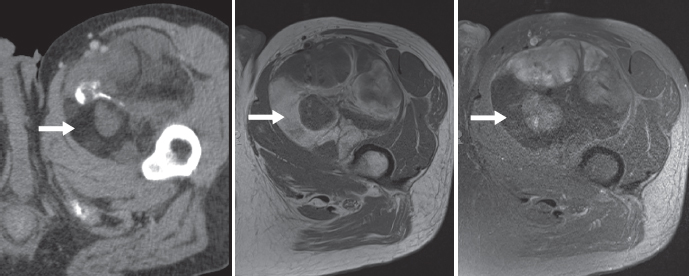
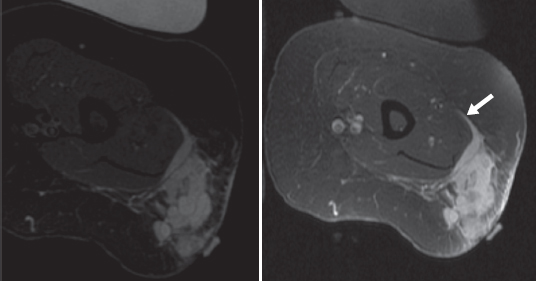
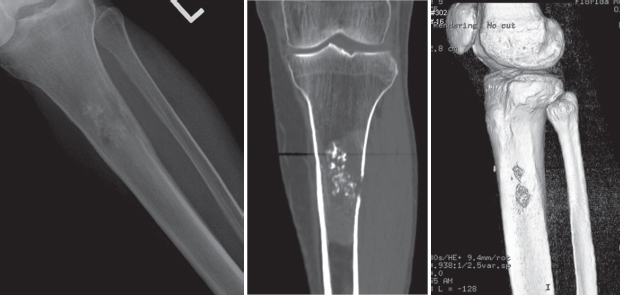
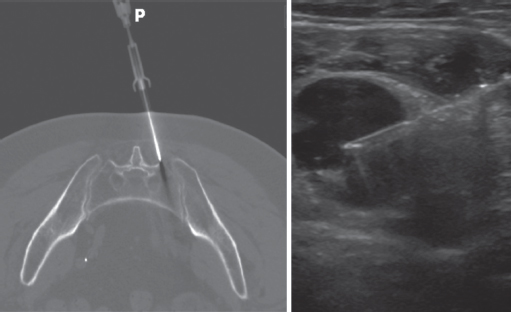
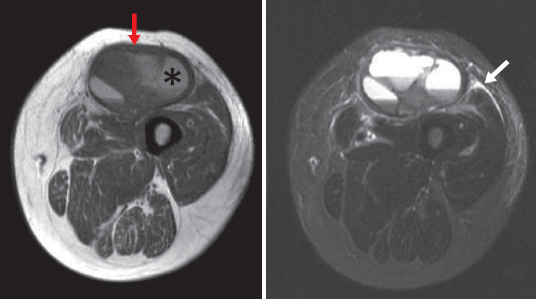
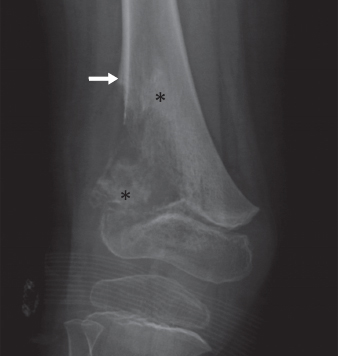
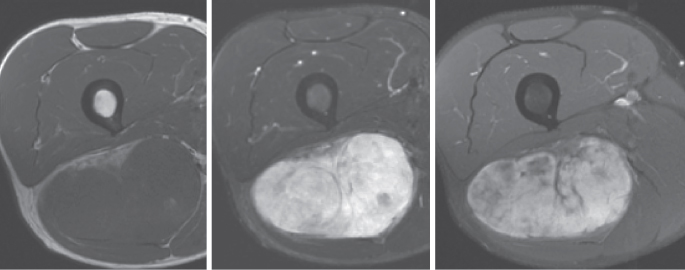
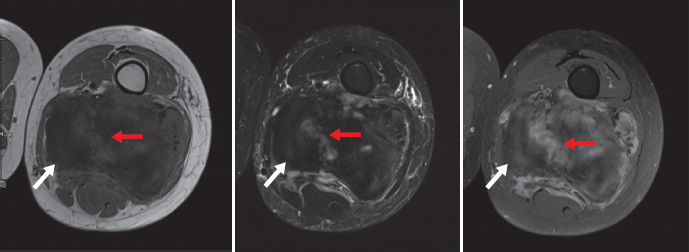
CLINICAL AND RADIOGRAPHIC FEATURES 3.2 Imaging of Soft Tissue and Bone Tumors All specimen interpretations should be performed with as much clinical information as possible. Even nominal information such as patient age, gender, and biopsy site can be invaluable in helping to include or exclude specific entities. The patient’s previous history and a family history of malignancy can often provide valuable insight into the type of tumor for any given patient. Many tumors occur preferentially in selected populations. For example, infantile fibrosarcoma, fibrous hamartoma of infancy, and lipoblastoma are lesions that occur almost exclusively in the pediatric population. Likewise, many tumors are site restricted, and the presence of a tumor in a typical location can be helpful in the formulation a differential diagnosis (Table 3.1.1). Chordoma and elastofibroma are just two examples of lesions that would be unlikely diagnostic choices if the tumor was not located in a specific location. Patients with soft tissue sarcoma tend to present with vague signs and symptoms. Because sarcomas are often located in deep locations (the most common location is the deep compartment of the thigh), they can become very large before the patient becomes aware of a limb asymmetry. Similarly, retroperitoneal lesions can become very large before the patient notices an increase in abdominal girth. It is not uncommon for some rather indolent tumors (atypical lipomatous tumor is a classic) to declare their presence when a patient loses a significant amount of weight from dieting. Bone tumors may present with pain and swelling, particularly if malignant. Bone lesions that cause significant structural weakness (fibrous dysplasia, nonossifying fibroma, and cystic lesions) can present with deformity or fracture of the involved region. Pathologic fracture is a common presentation for rapidly growing and destructive lesions. The growth characteristics of a tumor, as well as the presence or absence of associated pain, can also be important diagnostic clues. These features are particularly important in the diagnosis of primary bone tumors. For example, the pain pattern associated with osteoid osteoma (nocturnal and relieved with anti-inflammatory medication) is almost pathognomonic of this lesion. In addition, primary bone tumors are often centered on a particular region of the bone (metaphysis, epiphysis, or diaphysis). Knowledge of the site distribution of some of the most common bone tumors can help in formulating a differential diagnosis. Finally, simple laboratory tests can prove useful for diagnosis, particularly of bone tumors. The “brown tumor” of hyperparathyroidism, for example, can closely mimic a giant cell tumor. In this instance, a simple serum calcium or phosphate measurement can be helpful in confirming or excluding this specific diagnosis. Likewise, osteomyelitis is often in the clinical and radiographic differential diagnosis of a number of bone lesions, specifically in the pediatric population. An elevated sedimentation rate, although not in itself specific, often indicates infection and can be a useful piece of information. TABLE 3.1.1 Bone and Soft Tissue Tumors That Are Restricted to Specific Sites Lesion Site(s) Soft tissue lesions Elastofibroma Calcifying aponeurotic fibroma Inclusion body fibroma/infantile digital fibroma Nuchal fibroma Palmar/plantar fibromatosis Angiomyofibroblastoma Cellular angiofibroma Aggressive angiomyxoma Intimal sarcoma Subscapular region Palmar and plantar surfaces of hands and feet Distal digits Posterior neck/upper back Hands and feet Inguinal/genital region Inguinal/genital region Deep genital or inguinal region Heart and great vessels Bone lesions Chordoma Adamantinoma Osteofibrous dysplasia Sacrum, clivus, vertebral column Tibia Tibia, fibula 3.2 Imaging of Soft Tissue and Bone Tumors Jamie T. Caracciolo A close correlation between histopathologic and radiologic findings plays a critical role in accurate diagnosis of primary and secondary musculoskeletal neoplasms, including primary osseous tumors and soft tissue sarcomas. When the preoperative radiologic appearance of a tumor at diagnostic imaging, such as radiographs, CT, and MRI, closely correlates with the histopathologic findings at biopsy, a confident presurgical diagnosis will help direct and define patient management planning. When pathognomonic findings at imaging or pathology are not present, a review of the histopathologic findings in the light of pertinent radiologic findings is extremely useful. Certain imaging findings may help distinguish among pathologic diagnoses, which are difficult to differentiate microscopically when tumors have similar pathologic features (eg, smooth muscle and fibrous tumors of soft tissue which are spindle cells mainly). One other example is to determine if a small biopsy of a lipomatous tumor is truly an atypical lipomatous tumor and well differentiated liposarcoma. When correlated with specific MRI findings such as enhancing nodules and thick septations, a confident preoperative diagnosis of liposarcoma can be made. Similarly, pathologic distinction between enchondroma and low-grade chondrosarcoma can be difficult, but when deep scalloping or early cortical breakthrough are seen on x-rays, chondrosarcoma is the proper diagnosis (Figures 3.2.1 and 3.2.2). In some cases, the biopsy specimen may represent only a single component of an otherwise heterogeneous neoplasm composed of multiple differential cell types, such as several dedifferentiated neoplasms including dedifferentiated liposarcoma. Histopathologic correlation with findings at image-guided biopsy can demonstrate the corresponding site of biopsy or, alternatively, identify an optimal region for targeted tissue sampling (Figure 3.2.3). In yet other cases, both the histopathologic and radiologic findings are nonspecific, but still allow distinction between benign and malignant diseases. For example, biopsy may demonstrate a spindle cell neoplasm, that is not otherwise specified. At imaging, findings such as tumor size, location, enhancement, necrosis, and internal hemorrhage may suggest whether a tumor is benign or malignant. When close histopathologic and radiologic correlation are interpreted in the appropriate clinical context, including patient age, past medical history, and physical findings, accurate and actionable preoperative diagnosis of bony and soft tissue neoplasms is possible. The initial evaluation of a bony or soft tissue mass should attempt to determine whether a lesion appears to be indolent or aggressive, that is, benign or malignant (Figures 3.2.4 and 3.2.5). In many cases, further inspection of internal tumor composition at cross sectional imaging such as CT or MRI, which closely correlates with histopathologic findings, will allow for a more specific preoperative diagnosis or otherwise provide for a short list of differential diagnostic considerations. Many “clues” in the diagnostic evaluation, such as pattern of growth, surrounding edema, and internal necrosis, help suggest benignity versus malignancy. Meanwhile, identification of specific internal soft tissue elements or tumor matrix mineralization patterns may provide more specific diagnosis. In turn, imaging findings help direct patients to surveillance (follow-up) or further evaluation including image-guided or surgical biopsy. Certainly, determination of a preoperative histopathologic diagnosis is best established utilizing a multidisciplinary team approach. The first step in the workup of a suspected musculoskeletal neoplasm, particularly bone tumors, should include two-view radiographs of the affected area (note that radiographs do have significant utility for both bone and soft tissue tumors). Anteroposterior (AP) and lateral radiographs allow inspection of several important features of a bony lesion. Findings such as tumor margin, matrix, and periosteal reaction should initially suggest tumor aggressiveness or non-aggressiveness. Most primary (and secondary) bone tumors present as lytic, or lucent, lesions on x-rays. In these cases, radiographic features including margin and location within bone, periosteal reaction, fracture, or associated soft tissue mass should suggest tumor rate of growth (Figure 3.2.6). At the same time, further evaluation of the tumor matrix on plain films, seen as variable degrees and patterns of mineralization within the matrix of the tumor, often allows prediction of tumor pathology. For example, the matrix of cartilage-forming tumors typically includes punctate, curvilinear, and flocculent calcifications (Figure 3.2.7), whereas the matrix of most fibrous-forming neoplasms are void of mineralization and typically present with “ground-glass” radiolucency (Figure 3.2.8). Other x-ray findings, which help form the differential diagnosis or suggest specific histopathology, include pattern of tumor growth within a bone, peripheral (cortical) versus central (medullary) location, and reaction of host bone to the tumor (ie, sclerotic rim). Finally, integrating all available information on the films with relevant clinical information can help further narrow a differential diagnosis and, in some cases, predict histopathology. For example, a young male with a thigh mass presenting with a dense, sclerotic distal femoral lesion with spiculated periosteal reaction would be consistent with osteoblastic osteosarcoma. After radiographic evaluation, cross-sectional imaging, such as CT or MRI, is often performed in the initial diagnostic evaluation of bony and soft tissue neoplasms. CT and MRI demonstrate numerous separate and complementary findings, which help characterize musculoskeletal tumors. CT better demonstrates tumor mineralization, cortical involvement, and visualization of fractures, while being extremely useful in patient staging when necessary. MRI has improved soft tissue contrast compared to CT, allowing for differentiation of various soft tissue elements within a tumor (ie, chondroid, myxoid, or fibrous elements), which correlate with findings at gross tumor dissection and final tumor pathology. MRI of musculoskeletal neoplasms commonly includes T1-weighted, T2-weighted with and without fat suppression (or other fluid sensitive sequence such as short tau inversion recovery [STIR] imaging), and intravenous contrast-enhanced imaging. These sequences allow visualization of several findings that help differentiate benign and malignant neoplasms. Typical imaging characteristics of soft tissue sarcomas include large size, solid soft tissue elements demonstrating contrast enhancement, internal necrosis, hemorrhage, peripheral pseudocapsule, and surrounding peritumoral edema. Additionally, deep-seated tumors, defined by the investing fascia of the compartmental musculature in the extremities, carry greater risk of malignancy than superficial tumors, though there are superficial malignancies such as cutaneous leiomyosarcoma and dermatofibrosarcoma protuberans. Conversely, benign neoplasms tend to be small, homogeneous, and well-defined lesions without peritumoral edema. MRI can also demonstrate the soft tissue elements within a tumor, allowing for a more specific preoperative diagnosis. The presence of fat within a tumor, for example, would be consistent with a lipomatous neoplasm. Fat appears bright on both T1-weighted and T2-weighted imaging, while demonstrating signal suppression on fat saturation (FAT SAT) sequences (Figure 3.2.9). Myxomatous tissue demonstrates a very bright signal on T2-weighted imaging with variable degrees of intravenous (IV) contrast enhancement (Figure 3.2.10). Enhancement distinguishes myxoid tissue from areas of necrosis or cystic degeneration, which also are both T2-bright, but do not enhance. Fibrous tissues, such as within desmoid tumors, fibromatosis, and fibrosarcomas, typically demonstrates low, or dark, signal on both T1-weighted and T2-weighted imaging, corresponding with collagen deposition (Figure 3.2.11). Patterns of tumor growth may also help suggest a specific preoperative pathologic diagnosis. For example, indolent, slow-growing cartilaginous neoplasms of bone usually demonstrate cortical thickening or marginal (rim) sclerosis as the host bone attempts to limit tumor expansion. Cartilage tumors also commonly demonstrate a lobulated morphology, corresponding with cartilage lobules at pathology. Additionally, a cartilaginous matrix is high in water content and therefore characteristically has a bright signal on T2-weighted imaging, while also showing linear and peripheral enhancement along sites of chondrocytic viability/activity inbetween cartilage lobules. In contrast, fibrous neoplasms often demonstrate an infiltrative growth pattern arising from and extending along fascial planes (Figure 3.2.12). This infiltrative pattern may contribute to higher rates of local tumor recurrence. In conclusion, an accurate and specific preoperative diagnosis provides for proper consideration and selection of neo-adjuvant therapies, which have been shown to improve local tumor control rates, which, in turn, allow for limb-salvage procedures rather than amputation in most cases. The confidence and specificity of preoperative diagnosis is dependent on a close correlation between the histopathologic and radiologic findings. This is best achieved through an integrated, multidisciplinary group approach with expertise and experience in the diagnosis and management of musculoskeletal tumors. FIGURE 3.2.1 Enchondroma of the proximal humerus: Lateral radiograph demonstrates a lucent lesion with chondroid matrix without deep endosteal scalloping or cortical disruption consistent with enchondroma (inset: MRI shows lobulated T2-weighted bright medullary lesion). FIGURE 3.2.2 Low-grade chondrosarcoma of the proximal tibia: AP radiograph, coronal CT, and three-dimensional (3-D) volume rendering demonstrate a lucent medullary lesion with flocculent chondroid mineralization and deep lateral endosteal scalloping including cortical breakthrough seen clearly on CT. FIGURE 3.2.3 Examples of image-guided biopsies: CT-guided biopsy of sacral bone lesion and ultrasound-guided biopsy of lymphadenopathy. FIGURE 3.2.4 Characteristics of a benign soft tissue mass: MRI demonstrates a small, well-defined rounded, homogeneous palpable right axillary mass; magnified T2-w image demonstrates the “string sign” consistent with benign peripheral nerve sheath tumor. FIGURE 3.2.5 Characteristics of a malignant soft tissue mass: MRI demonstrates a large, heterogeneous mass with internal hemorrhage (asterisk), thick pseudocapsule (red arrow), and peritumoral edema (white arrow) proven to be undifferentiated pleomorphic sarcoma. FIGURE 3.2.6 Skeletally immature patient with osteosarcoma of the distal right femur: AP radiograph demonstrates an ill-defined lytic and sclerotic lesion with lateral cortical destruction, soft tissue mass, and Codman’s triangle (arrow); areas of increased density (black asterisks) correspond with osteoid matrix. FIGURE 3.2.7 An 18-year-old male with chondroblastoma of the left humerus: AP radiograph, coronal CT, and T2-weighted MRI demonstrate a well-defined, geographic lytic lesion with marginal sclerosis (arrow) involving the humeral epiphysis with stippled and flocculent mineralization and increased T2-weighted signal intensity; imaging appearance, age, and location are consistent with chondroblastoma. FIGURE 3.2.8 Fibrous dysplasia of the radius: AP and lateral radiographs demonstrate multiple well-defined, mildly expansile central medullary lucent lesions without mineralization, rather with hazy “ground-glass” appearance consistent with fibrous dysplasia. FIGURE 3.2.9 Fat-containing proximal thigh mass: Axial CT, T1-weighted, and fat-suppressed contrast-enhanced MRI demonstrate a soft tissue mass with internal fat indicative of a lipomatous neoplasm. Fat is seen as areas of low density on CT, while these same areas follow the signal intensity of subcutaneous fat on MRI sequences (arrows). Also note enhancing nonadipocytic soft tissue elements and calcifications elsewhere within this dedifferentiated liposarcoma. FIGURE 3.2.10 Myxomatous soft tissue mass of the posterior right thigh: Axial T1-weighted, fat-suppressed T2-weighted, and contrast-enhanced MRI demonstrate a large soft tissue mass with very bright T2-weighted signal similar to fluid, but with avid enhancement consistent with myxoid tissue. Note subtle bright foci on T1-weighted imaging indicating internal fat within this myxoid liposarcoma. FIGURE 3.2.11 Fibrous mass of the posterior thigh: Axial T1-weighted, fat-suppressed T2-weighted, and contrast-enhanced MRI demonstrate a large mass, which is predominantly dark on all pulse sequences corresponding with diffuse fibrous/collagen deposition (white arrows); note T2-bright and enhancing sites of active tumor laying down fibrous matrix (red arrows). FIGURE 3.2.12 Mass with infiltrative pattern of growth: Axial fat-suppressed T2-weighted and contrast-enhanced MR images demonstrate a T2-weighted bright lateral thigh mass with avid enhancement indicative of a myxoid neoplasm with nodular and infiltrative growth pattern including extension along the investing fascia (arrow) proven to be myxofibrosarcoma.

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Clinical and Radiographic Features