Chondroblastoma
G. Petur Nielsen, MD
Andrew E. Rosenberg, MD
Key Facts
Terminology
Calcifying giant cell tumor, Codman tumor, epiphyseal chondromatous giant cell tumor
Uncommon benign cartilage neoplasm
Clinical Issues
Age range: 10-25 years
Skeletally immature individuals
Pain
Usually treated by curettage
Local recurrence rate: 14-18%
Pulmonary metastases from histologically benign chondroblastomas are well-recognized phenomenon
Image Findings
Manifests as intramedullary, well-defined tumor
Contains scalloped borders, sclerotic rim, and internal calcifications
Macroscopic Features
Gritty
Grayish white
Hemorrhagic cystic areas common
Microscopic Pathology
Densely cellular
Composed of admixture of mononuclear chondroblasts and multinucleated osteoclast-type giant cells
Chondroblasts grow in sheets
Matrix generally consists of poorly formed hyaline cartilage
TERMINOLOGY
Abbreviations
Chondroblastoma (CBA)
Synonyms
Calcifying giant cell tumor
Codman tumor
Epiphyseal chondromatous giant cell tumor
Definitions
Benign cartilage-producing neoplasm composed of chondroblasts that typically arises in epiphysis of skeletally immature individuals
ETIOLOGY/PATHOGENESIS
Unknown
Presumably develops from mutations in intraosseous mesenchymal stem cells
CLINICAL ISSUES
Epidemiology
Incidence
Accounts for approximately 1% of primary bone tumors
Responsible for < 3% of primary benign bone tumors
In individuals younger than 18 years, incidence is 1.18 per million
Age
Affected individuals are typically skeletally immature, with open growth plates, between ages 10-25 years
Rare in young children and elderly
Gender
More common in males
M:F = 2:1
Site
Arises in any bone that develops from endochondral ossification
Typically develops in epiphysis of long tubular bones (66%)
Most common sites are distal and proximal femur, followed by proximal tibia and proximal humerus
Approximately 37% limited to epiphysis
About 65% involve epiphysis and extend into metaphysis
Vast majority are centered in medullary cavity; intracortical and surface tumors are rare
Apophyseal origin is less frequent (25%)
Usually originates in greater trochanter of femur and greater tuberosity of humerus
Bones of hands and feet affected in 10%
Other locations include talus, calcaneus, patella, acetabulum, iliac crest, temporal bone, and skull base
Tumors arising in metaphyseal and diaphyseal locations are rare
Almost all chondroblastomas are solitary
Multifocal chondroblastoma is very rare
Chondroblastomas in adults develop in unusual locations, such as skull and facial bones
Presentation
Pain
Tender on palpation
Swelling
Limitation of range motion
Limping
Joint stiffness
Pathologic fracture through articular surface
Natural History
Slow enlargement associated with increase in severity of pain and other symptoms
May locally recur following curettage or incomplete resection
Metastases develop in < 1% of patients
Usually follows multiple recurrences or patients who present with pathologic fracture
Malignant transformation very rare
Treatment
Curettage and packing with bone graft
Percutaneous radiofrequency heat ablation in appropriate cases
Resection in selected cases
Radiation in tumors that are in critical anatomic locations, such as skull base
Prognosis
Local recurrence rate: 14-18%
Higher recurrence rate in tumors arising in temporal bone and ribs
Local recurrences usually develop within 1st 3 years following curettage
May be detected after much longer time interval
Pulmonary metastases from histologically benign chondroblastomas are well-recognized phenomenon
Metastases are slowly progressive
Maintain histologic appearance of benign chondroblastoma
Rarely fatal and can be treated with resection
Usually develop > 5 years after primary diagnosis
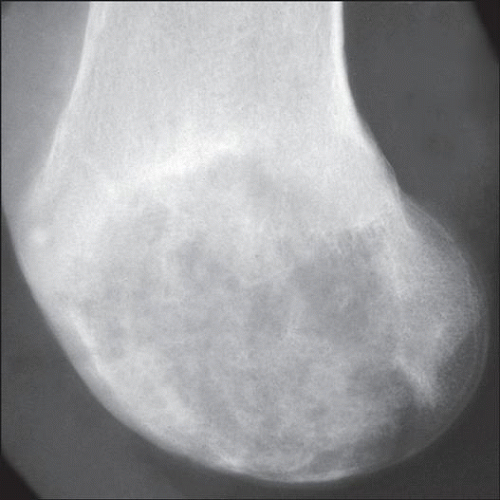
IMAGE FINDINGS
Radiographic Findings
Intramedullary, eccentric or central, well-defined tumor with sclerotic margins
Predominately radiolucent but frequently contains scattered punctate calcifications
May scallop cortex or result in its destruction
Neighboring marrow is altered by edema
Secondary aneurysmal bone cyst-like changes may cause extensive expansion of bone and periosteal reaction, mimicking a more aggressive neoplasm
In chondroblastoma with extensive aneurysmal bone cyst-like changes, it can sometimes be difficult to identify features of underlying primary chondroblastoma
MR Findings
Chondroblastoma has low or intermediate signal intensity on T1-weighted image and may be obscured by surrounding edema
Tumor has high or variable intensity on T2-weighted image
Prominent edema in marrow and soft tissue
Joint effusion is common
CT Findings
Chondroblastoma is oval, well demarcated, and shows internal calcifications
Bone Scan
Marked increased activity on bone scan
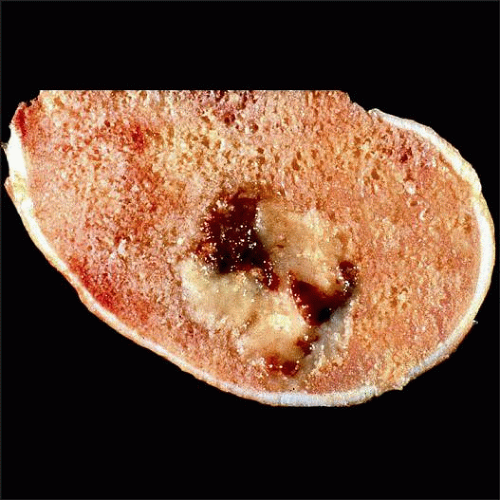
MACROSCOPIC FEATURES
General Features
Well circumscribed, round or oval, red-gray-white, and gritty
Hemorrhagic cystic areas common and are prominent in tumors with secondary aneurysmal bone cyst-like changes
Size
Range in size from 1-19 cm (average: 3.6 cm)
85% are ≤ 5 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Densely cellular with sharp margins and surrounding reactive bone
Composed of admixture of mononuclear chondroblasts and multinucleated osteoclast-type giant cells
Chondroblasts grow in sheets, have eosinophilic cytoplasm delineated by well-defined cell borders
Nuclei are eccentric, reniform or coffee-bean-shaped, similar to nuclei in Langerhans cell histiocytosis
Mitotic activity and regional necrosis may be present, the latter especially in calcified areas
Chondroid matrix can be pink or basophilic and sometimes resemble woven bone
Well-formed hyaline cartilage uncommon
Mineralization of matrix surrounding individual cells imparts characteristic “chicken wire” pattern
Osteoclast-type giant cells scattered throughout tumor, usually most numerous in areas of matrix production and hemorrhage
Osteoclast-type giant cells are nonneoplastic and recruited by chondroblasts
Chondroblastoma abutting temporomandibular joint frequently shows intracytoplasmic hemosiderin deposition mimicking tenosynovial giant cell tumor
Some cases reported in literature likely represent tenosynovial giant cell tumor
Necrosis in fractured tumors and in areas of prominent calcification
Vascular invasion uncommon
Concept of “malignant” chondroblastoma is controversial
Some pathologists believe that most of these tumors represent either misdiagnosis or radiation-induced sarcoma
Term “aggressive chondroblastoma” is used for tumors that histologically have features of chondroblastoma but show destructive growth pattern radiographically
Tumor in metastatic deposits similar to that of primary and frequently surrounded by rim of reactive bone
ANCILLARY TESTS
Cytology
Clonal abnormalities especially involving chromosomes 5 and 8 have been identified
Recent study has shown a balanced t(5;17) in chondroblastoma in chondroblasts but not osteoclasttype giant cells
Immunohistochemistry
Chondroblasts express S100 protein and SOX9
Tumor cells may stain for muscle actin, keratin, and epithelial membrane antigen
Osteoclast-type giant cells stain for histiocytic markers
RANKL, a stimulator of osteoclast production and activity, is expressed by tumor cells
By this mechanism, osteoclasts are recruited into tumor and produce resorption and lysis of underlying bone
Extracellular matrix stains for collagen type II
DIFFERENTIAL DIAGNOSIS
Chondromyxoid Fibroma
Usually arises in metaphysis and not epiphyses
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree