Patient Story
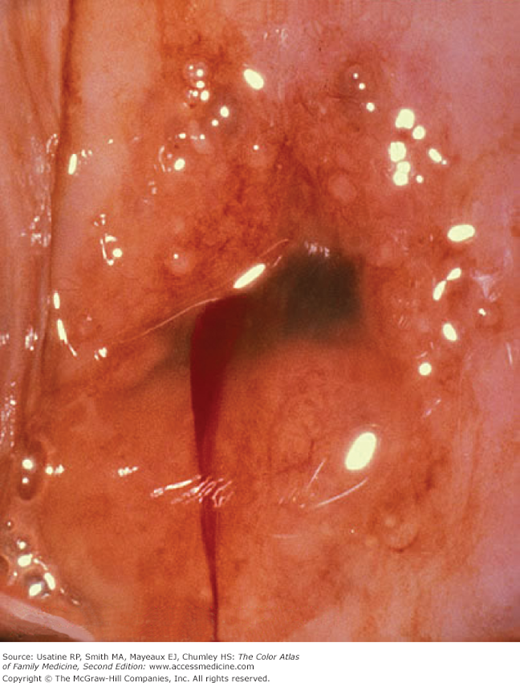
A 17-year-old girl presents to the sexually transmitted disease (STD) clinic because her boyfriend was diagnosed with a Chlamydia urethritis. Both she and her boyfriend admit to having had sexual partners in the past before starting to be sexually active with each other. On physical examination, there is ectopy and some mucoid discharge (Figure 85-1). The cervix bled easily while obtaining discharge and cells for a wet mount and genetic probe test. The wet mount showed many white blood cells (WBCs) but no visible pathogens. The patient was treated with 1 g of azithromycin taken in front of a clinic nurse. She was sent to the laboratory for rapid plasma reagin (RPR) and HIV tests and given a follow-up appointment in 1 week. The genetic probe test was positive for Chlamydia and all the other examinations were negative. This information was given to the patient on her return visit and safe sex was discussed.
Introduction
Chlamydia trachomatis causes genital infections that can result in pelvic inflammatory disease (PID), ectopic pregnancy, and infertility. Asymptomatic infection is common among both men and women so healthcare providers must rely on screening tests to detect disease. The Centers for Disease Control and Prevention (CDC) recommends annual screening of all sexually active women ages 25 years and younger, and of older women with risk factors, such as having a new sex partner or multiple sex partners.1
Epidemiology
- A very common STD, Chlamydia is the most frequently reported infectious disease in the United States (excluding human papillomavirus [HPV]).1 An estimated 1.2 million cases are reported to the CDC annually in the United States.2
- The World Health Organization (WHO) estimates there are 140 million cases of Chlamydia trachomatis infection worldwide every year.3
- The CDC estimates screening and treatment programs can be conducted at an annual cost of $175 million. Every dollar spent on screening and treatment saves $12 in complications that result from untreated Chlamydia.4
- It is common among sexually active adolescents and young adults.5 As many as 1 in 10 adolescent girls tested for Chlamydia is infected. Based on reports to the CDC provided by states that collect age-specific data, teenage girls have the highest rates of chlamydial infection. In these states, 15- to 19-year-old girls represent 46% of infections and 20- to 24-year-old women represent another 33%.4
Etiology and Pathophysiology
- C. trachomatis is a small Gram-negative bacterium with unique biologic properties among living organisms. Chlamydia is an obligate intracellular parasite that has a distinct life-cycle consisting of two major phases: The small elementary bodies attach and penetrate into cells, and the metabolically active reticulate bodies that form large inclusions within cells.
- It has a long growth cycle, which explains why extended courses of treatment are often necessary. Immunity to infection is not long-lived, so reinfection or persistent infection is common.
- The infection may be asymptomatic and the onset often indolent. It can cause cervicitis, endometritis, PID, urethritis, epididymitis, neonatal conjunctivitis, and pediatric pneumonia. Of exposed babies, 50% develop conjunctivitis and 10% to 16% develop pneumonia.1
- Chlamydia infections may lead to reactive arthritis, which presents with arthritis, conjunctivitis, and urethritis (Chapter 155, Reactive Arthritis). Past or ongoing C. trachomatis infection may be a risk factor for ovarian cancer.6,7
- Up to 40% of women with untreated Chlamydia will develop PID. Undiagnosed PID caused by Chlamydia is common. Of those with PID, 20% will become infertile; 18% will experience debilitating, chronic pelvic pain; and 9% will have a life-threatening tubal pregnancy. Tubal pregnancy is the leading cause of first-trimester, pregnancy-related deaths in American women.4
Risk Factors
Diagnosis
- The cervix is inflamed, friable, and may bleed easily with manipulation. The cervix may show ectopy (columnar cells on the ectocervix). The discharge is usually mucoid or mucopurulent (Figure 85-1).
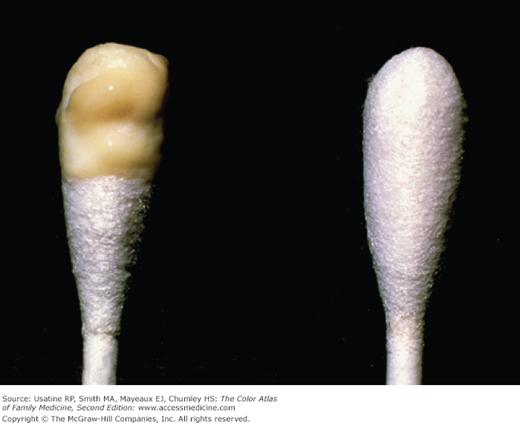
- Swab test—A white cotton-tip applicator is placed in the endocervical canal and removed to view. A visible mucopurulent discharge constitutes a positive swab test for Chlamydia (Figure 85-2). This is not specific for Chlamydia as other genital infections can cause a mucopurulent discharge, and is not recommended for diagnosis.
- A significant proportion of patients with Chlamydia are asymptomatic, providing a reservoir for infection. All pregnant women and sexually active women younger than 25 years of age should be screened with routine examinations. A wet prep is usually negative for other organisms. Only WBCs and normal flora are seen.
- Chlamydia cannot be cultured on artificial media because it is an obligate intracellular organism. Tissue culture is required to grow the live organism. When testing for Chlamydia, a wood-handled swab must not be used, as substances in wood may inhibit Chlamydia organism. Culture has sensitivity of 70% to 100% and a specificity of almost 100%, which makes it the gold standard.1
- The enzyme-linked immunosorbent assay (ELISA) technique (Chlamydiazyme) has a sensitivity of 70% to 100% and a specificity of 97% to 99%.5 Fluorescein-conjugated monoclonal antibodies test (MicroTrak) has a sensitivity of 70% to 100% and a specificity of 97% to 99%.5
- C. trachomatis

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree