Chapter 13 Chest Inspection, Palpation, and Percussion
Generalities
2 What is the usual sequence in a typical pulmonary exam?
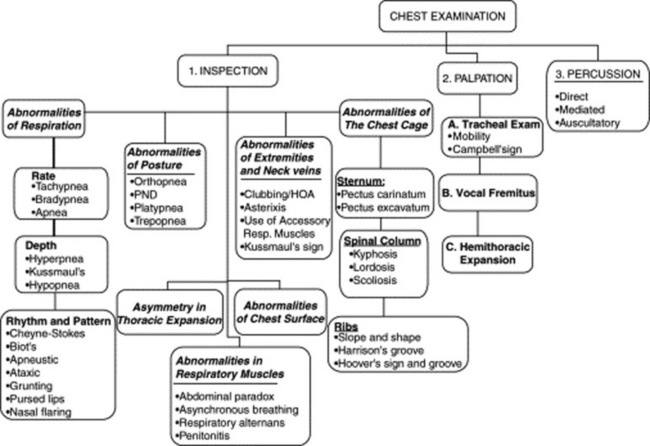
The patient usually remains seated, with the physician moving from front to back and sides. Initial assessment includes an evaluation of effort, rate, and depth of respiration. It also should identify any wheeze, or grunt, or noisy sound that might be audible without the need of a stethoscope. Sequential inspection of the anterior, posterior, and lateral chest should then be carried out. Finally, palpation, percussion, and auscultation complete the exam. The examination should be thorough and go from the chest surface toward the inner structures (Fig. 13-1).
A. Chest Inspection
(1) Abnormalities of Respiration
Abnormalities in the Depth of Respiration
21 Who was Kussmaul?
Adolf Kussmaul (1822–1902) was a graduate of Heidelberg and Würzburg (where he studied under Virchow) and a part-time German Army surgeon. He was the first to describe periarteritis nodosa and progressive bulbar paralysis. He also was the first to attempt gastroesophagoscopy, pleural tapping, and peritoneal lavage. His name is linked to the respiration of patients with metabolic acidosis, the clinical description of pericarditis, pulsus paradoxus, aphasia, and, of course, Kussmaul’s sign, the inspiratory increase in jugular venous pressure (and distention) seen in patients with obstruction to right-sided venous return (see Chapter 10, questions 115–118). A meticulous and precise man famous for complaining that none of his colleagues could write good German, Kussmaul contributed satirical poems to a weekly magazine under the pseudonym of Gottlieb Biedermeier, an imaginary and unsophisticated poet who eventually came to symbolize the values and tastes of the early 19th-century German bourgeois: reliable, hard-working, but boringly unimaginative (like in the Biedermeier style of furniture. “Bieder” is German for “everyday, plain” while “Meier,” or Meyer, is a common German last name).
22 What is hypopnea?
It is shallow respiration, usually indicative of impending respiratory failure or obesity-hypoventilation (Pickwickian syndrome). In this regard, hypopnea is often associated with periods of apnea (see question 17).
Abnormalities in Rhythm and Pattern of Respiration
23 What are the main abnormalities in respiratory rhythm?
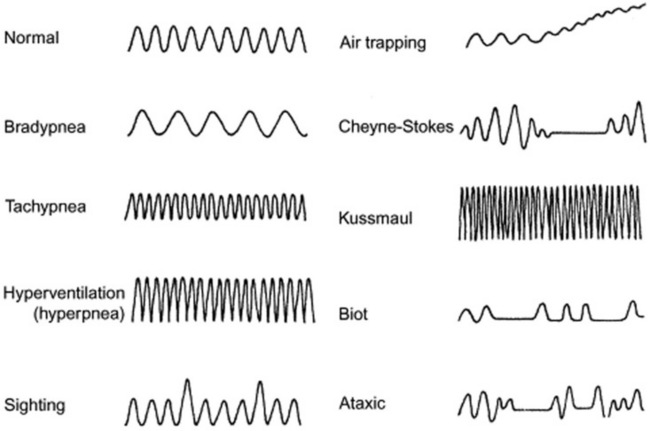
They are many, and usually the result of disruption in the neurogenic control of the respiratory pump. Hence, they are often seen in comatose patients. Thus, they are valuable to recognize because they may help localizing the site of the neurologic lesion (see Fig. 13-2). Moving downward in a rostrocaudal fashion, from the uppermost to the lowermost neurologic center, the most common abnormalities of respiratory rhythm are (1) Cheyne-Stokes respiration, (2) Biot’s respiration, (3) apneustic breathing, (4) central hyperventilation, and (5) ataxic (agonal) respiration.
26 What is the clinical significance of Cheyne-Stokes?
 It may be encountered in normal people as a result of aging or simply sleep.
It may be encountered in normal people as a result of aging or simply sleep.
 It also can be seen in normal individuals who recently moved to high altitudes, where environmental hypoxia leads to a heightened CO2 response of the respiratory centers.
It also can be seen in normal individuals who recently moved to high altitudes, where environmental hypoxia leads to a heightened CO2 response of the respiratory centers.
 The classic association, however, is with congestive heart failure, where Cheyne-Stokes is found in as many as one third of cases, reflecting worse function and prognosis. The reduced cardiac output of these patients leads to a lag between alveolar CO2 and the arterial CO2 delivered to the medulla. Hence, low alveolar CO2 is reflected much later in the blood that bathes the medulla. This asynchrony between alveoli and medulla, coupled to higher sensitivity of the respiratory centers to CO2, eventually leads to the hyperpnea-hypopnea-apnea cycle.
The classic association, however, is with congestive heart failure, where Cheyne-Stokes is found in as many as one third of cases, reflecting worse function and prognosis. The reduced cardiac output of these patients leads to a lag between alveolar CO2 and the arterial CO2 delivered to the medulla. Hence, low alveolar CO2 is reflected much later in the blood that bathes the medulla. This asynchrony between alveoli and medulla, coupled to higher sensitivity of the respiratory centers to CO2, eventually leads to the hyperpnea-hypopnea-apnea cycle.
 Cheyne-Stokes also can be seen in various neurologic disorders (such as meningitis, bilateral or unilateral cerebral infarctions/hemorrhage, and traumatic brain stem or supratentorial damage) in which the underlying mechanism is heightened sensitivity of the respiratory centers to carbon dioxide stimulations. As a result, any increase in CO2 blood levels leads to excessive hyperventilation, until the CO2 bottoms out and respiration ceases completely. Eventually, the apnea-induced increase in CO2 leads to another phase of hyperpnea, and the cycle starts anew.
Cheyne-Stokes also can be seen in various neurologic disorders (such as meningitis, bilateral or unilateral cerebral infarctions/hemorrhage, and traumatic brain stem or supratentorial damage) in which the underlying mechanism is heightened sensitivity of the respiratory centers to carbon dioxide stimulations. As a result, any increase in CO2 blood levels leads to excessive hyperventilation, until the CO2 bottoms out and respiration ceases completely. Eventually, the apnea-induced increase in CO2 leads to another phase of hyperpnea, and the cycle starts anew.
28 Who were Cheyne and Stokes?
William Stokes (1804–1878) was instead a bona-fide Irishman and the son of the anatomy professor who had succeeded John Cheyne at the College of Surgeons School in Ireland. Although lacking in formal education (his father wanted to protect him from a society that did not abide by the scriptures), Stokes eventually went to Edinburgh, where he received his doctor of medicine in 1825. In Scotland, he learned of Laënnec and his recent invention, the “cylinder.” He soon became so enamored of this little tool that he even wrote an introductory book about it, the first of its kind in the English language. In fact, Stokes was such a vocal advocate for the use of stethoscopy that he provoked quite a few reactions (and even some sarcasm) among his colleagues. Still, he was a well-liked physician, who worked among the poor during the Dublin typhus epidemic in 1826 (he even contracted the disease but survived) and then again during the subsequent cholera epidemic. His name is linked not only to the eponymous pattern of respiration but also to Stokes-Adams syncope, which the Irish surgeon Robert Adams had described in 1827 and which Stokes included in his 1854 book, Diseases of the Heart and Aorta. Of course, the Italian Morgagni had preceded them both by describing the condition almost 100 years before (see Chapter 11, question 14).
29 What other abnormalities in rhythm are worthy of recognition? What is their significance?
 Biot’s respiration is a variant of Cheyne-Stokes, insofar as it is a succession of hyperpneas/hyperventilations and apneas, but without the typical crescendo-decrescendo pattern, the abrupt beginning, and the regularity. It is also less common than Cheyne-Stokes. Biot’s is usually observed in patients with either meningitis or medullary compression. Hence, it carries a worse prognosis, usually resulting in complete apnea and cardiac arrest.
Biot’s respiration is a variant of Cheyne-Stokes, insofar as it is a succession of hyperpneas/hyperventilations and apneas, but without the typical crescendo-decrescendo pattern, the abrupt beginning, and the regularity. It is also less common than Cheyne-Stokes. Biot’s is usually observed in patients with either meningitis or medullary compression. Hence, it carries a worse prognosis, usually resulting in complete apnea and cardiac arrest.
 Apneustic breathing is a peculiar pattern of respiration, characterized by a deep inspiratory phase followed by a breath-holding period and a rapid exhalation. It is typical of brain stem (pons) lesions.
Apneustic breathing is a peculiar pattern of respiration, characterized by a deep inspiratory phase followed by a breath-holding period and a rapid exhalation. It is typical of brain stem (pons) lesions.
 Central hyperventilation is often encountered in patients with midbrain/upper pontine lesions. It is an ongoing pattern of hyperpnea and tachypnea (i.e., deep and rapid respirations), which tends to be different from Kussmaul’s respiration, insofar as it is not as fast, but usually deeper.
Central hyperventilation is often encountered in patients with midbrain/upper pontine lesions. It is an ongoing pattern of hyperpnea and tachypnea (i.e., deep and rapid respirations), which tends to be different from Kussmaul’s respiration, insofar as it is not as fast, but usually deeper.
 Ataxic ventilation: From the Greek a- (lack of) and taxis (order), this is a totally anarchic respiratory rhythm—a sort of fibrillation of the respiratory centers, with back-and-forth shifts from hyper- to hypo-ventilation, and from hyperpnea to hypopnea, all intermingled with periods of apnea. It is seen in patients with damage to the medulla, typically preceding death. Hence the term, agonal respiration.
Ataxic ventilation: From the Greek a- (lack of) and taxis (order), this is a totally anarchic respiratory rhythm—a sort of fibrillation of the respiratory centers, with back-and-forth shifts from hyper- to hypo-ventilation, and from hyperpnea to hypopnea, all intermingled with periods of apnea. It is seen in patients with damage to the medulla, typically preceding death. Hence the term, agonal respiration.
31 What is the clinical significance of a grunting respiration?
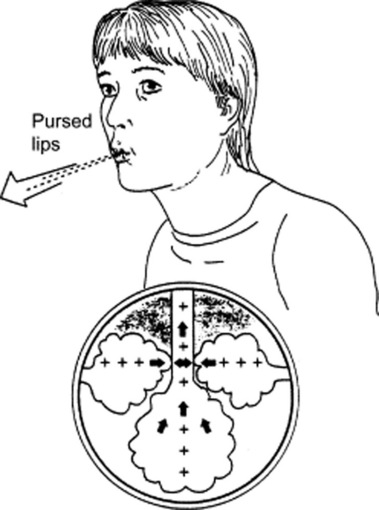
Very much the same as in Laënnec’s days. It can still be heard in adults with respiratory muscle fatigue (and impending arrest), but nowadays it is much more frequent in children, where it usually presents as a short and low-pitched noise produced by forced expiration against a closed glottis. The “grunt” is due to the sudden opening of the glottis and the loud rush of air from the larynx. Its physiology (and significance) is akin to pursed-lip respiration (see below, questions 32 and 33), insofar as it leads to an increase in expiratory airway pressure, which then acts as a mechanical splint against alveolar collapse, increasing tidal volume and oxygenation while decreasing respiratory rate and CO2. An increased intra-alveolar pressure also has a positive effect against transudation of fluid in patients with pulmonary edema, and thus it is often observed during acute episodes of left ventricular failure.
32 What is pursed-lip respiration?
Another respiratory pattern, typically seen in obstructive lung disease—usually emphysema (Fig. 13-3). Given the alveolar hyperinflation (and reduced lung elasticity) of COPD, patients are at risk for expiratory airway closure and air-trapping. Hence, they resort to pursed lip exhalation, as if they were inflating a balloon. This increases intra-airway pressure, thus inducing auto-PEEP (positive end-expiratory pressure). It is often accompanied by an expiratory wheeze or grunt.
39 And what about patients with COPD?
In COPD (which often presents with apical bullae), an upright position improves not only gas exchange but also lung mechanics (because of the increased stretch of accessory respiratory muscles). Hence, COPD patients often tend to prop themselves up, so that they can better use their respiratory muscles. They do so by clasping the side of the bed or pushing with the elbows over the thighs (see question 5, Dahl’s sign).
47 What is the clinical significance of platypnea?
 Multiple recurrent pulmonary emboli (which, because of gravity, tend to involve primarily the bases)
Multiple recurrent pulmonary emboli (which, because of gravity, tend to involve primarily the bases)
 Pleural effusion (which can cause bibasilar atelectasis) or bibasilar pneumonia
Pleural effusion (which can cause bibasilar atelectasis) or bibasilar pneumonia
 Cirrhosis (which often has arteriovenous shunting at the lung bases)
Cirrhosis (which often has arteriovenous shunting at the lung bases)
 Intrapulmonary right-to-left shunt, such as an arteriovenous malformation, often basilar in location
Intrapulmonary right-to-left shunt, such as an arteriovenous malformation, often basilar in location
 Intracardiac right-to-left shunt, usually due to an atrial septal defect. This produces platypnea only when associated with an increase in pulmonary resistances, as in cases of pleurocardial/pericardial effusion or status post lobectomy/pneumonectomy. An upright position will reduce the shunt by redirecting blood toward the atrial septum and by possibly increasing pressure over the right atrium. A supine posture will have instead the opposite effect.
Intracardiac right-to-left shunt, usually due to an atrial septal defect. This produces platypnea only when associated with an increase in pulmonary resistances, as in cases of pleurocardial/pericardial effusion or status post lobectomy/pneumonectomy. An upright position will reduce the shunt by redirecting blood toward the atrial septum and by possibly increasing pressure over the right atrium. A supine posture will have instead the opposite effect.
63 What are the main chest cage abnormalities?
 If the spine is affected, the abnormalities may be on the sagittal or frontal plane.
If the spine is affected, the abnormalities may be on the sagittal or frontal plane.
 If the sternum is involved, the two most common abnormalities are pigeon chest and barrel chest. Both may alter lung mechanics severely enough to reduce lung function.
If the sternum is involved, the two most common abnormalities are pigeon chest and barrel chest. Both may alter lung mechanics severely enough to reduce lung function.
 If ribs are involved, the most common abnormalities concern costal slope and shape.
If ribs are involved, the most common abnormalities concern costal slope and shape.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree