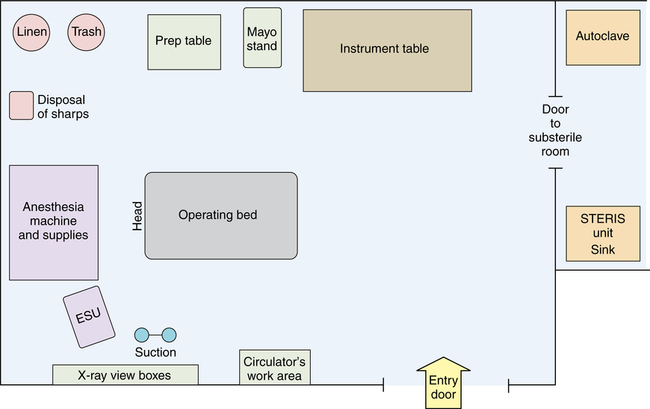
Chapter 12 After studying this chapter, the learner will be able to: • Describe how a room is prepared for the first case of the day. • Describe how a room is cleaned and prepared between patients. • Describe how a room is terminally cleaned at the end of the day. AORN has established standards and recommended practices for cleaning and maintaining optimal cleanliness in the perioperative environment. The recommendations include but are not limited to the following: 1. All patients are entitled to a clean environment for their surgical procedures. 2. Any contamination encountered during a surgical procedure should be contained and confined. 3. Between-case clean up should reestablish the cleanest environment possible for the next patient. 4. Procedure rooms and utility areas should be cleaned daily. 5. A schedule should be in place for routine cleaning of all areas and equipment in the surgical department. 6. All environmental sanitation processes should be defined by facility policy and procedure. The duties of the scrub person and circulating nurse are many and varied as they prepare for the arrival of the patient in the OR. They are responsible for the cleanliness of the environment preoperatively, intraoperatively, and postoperatively so that the potential for contamination of the patient is kept to a minimum. They prepare and maintain the sterile field, work within it, and then break it down for terminal cleaning. These activities are performed in specific steps to minimize the risk of infection and maximize the use of time and supplies. Standardization is in the best interest of the patient and the personnel performing the cleanup.1,2 A visual inspection of the room and its contents should be performed by the team before bringing in supplies for a case. Basic room contents should include the OR bed, anesthesia machine and supplies, electrosurgical unit (ESU), instrument table, preparation (prep) table, Mayo stand, suction apparatus, and receptacles for biohazard and regular trash, and reusable woven fabrics (Fig. 12-1). Other tables and equipment are added as needed. 1. Remove unnecessary tables and equipment from the room. Arrange the appropriate furniture in an organized manner away from the traffic pattern. Some head and neck procedures require the OR bed to be oriented in a sideways direction to provide working space for the anesthesia provider. 2. Damp-dust (with a facility-approved disinfectant solution and lint-free cloth) the overhead operating light, articulated arms, furniture, flat surfaces, and all portable or mounted equipment. Avoid dry-dusting because this sets dust aloft. Start at higher surfaces, and work down to lower levels because dust may fall from higher areas. 3. Damp-dust the tops and rims of the sterilizer and/or washer-sterilizer and the countertops in the substerile room adjacent to the OR. 4. Visually inspect the room for dirt and debris. The floor may need to be damp-mopped. 1. Patients with known respiratory-borne disease (i.e., rubeola, varicella, tuberculosis) may deposit microorganisms in the environment. In addition to routine environmental decontamination, the air exchanges should be 99% complete before the next patient is brought into the room. This may take 20 to 30 minutes on a 15- to 20-air change per hour cycle. Staff should wear appropriate filtration masks during room cleaning.a 2. Patients with known endospore-forming bacterial contamination (i.e., Clostridia or Bacillus spp.) may deposit bacterial endospores in the environment on inanimate objects known as fomites. These endospores have been shown to survive in the environment for 5 months and have been cultured in ORs 40 days after the patient has used the room. AORN recommended practices state that a hypochlorite-based disinfectant should be used for cleaning the environment.1,3 3. Patients with known or suspected transmissible spongiform encephalopathies (TSE) such as Creutzfeldt-Jakob disease (CJD) and new variant CJD may deposit prions in the environment. Prions are proteins found in neurologic tissue and fluids that cause fatal neurodegenerative diseases in humans and animals. Iatrogenic introduction of prion disease can happen if the patient is exposed to the protein during the surgical procedure by instrumentation or the environment. Prions are nonliving proteins that persist on surfaces and require special cleaning solutions. Disposable equipment, instruments, linens, and supplies should be used in the presence of known or suspected prion diseases.6 After a patient leaves the room, the immediate environment is cleaned and all surfaces are dried. Room cleanup between patients is directed at the prevention of cross-contamination.4 The cycle of contamination is from patient to environment and from environment to OR personnel and subsequent patients. Exposure to infectious waste is a hazard to everyone who encounters it. After each surgical procedure the environment should be made safe for the next patient to follow in that room. Institutional policies and procedures for routine room cleanup should be designed to minimize the OR team’s exposure to contamination during the cleaning process.2 The following are activities/responsibilities of the scrub person at the end of the case: 1. Push the Mayo stand and instrument table away from the operating bed (OR bed) as soon as the dressing is applied and the drapes are removed. Roll drapes off the patient from head to foot to prevent airborne contamination; do not pull them off. 2. Check drapes for towel clips, instruments, and other items. Be sure that no equipment is discarded with disposable drapes or sent to the laundry. Disposable drapes are placed in a red biohazard container for disposal. Soiled drapes, whether disposable or reusable, should be handled as little as possible and with minimum agitation to prevent gross microbial contamination of air by dispersal of lint and debris.
Care of the perioperative environment
Standards for cleanliness in the surgical environment
Establishing the surgical environment
Preliminary preparations
Before the first surgical procedure of the day
Room turnover between patients
Room turnover activities by the scrub person
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Care of the perioperative environment

 Website
Website