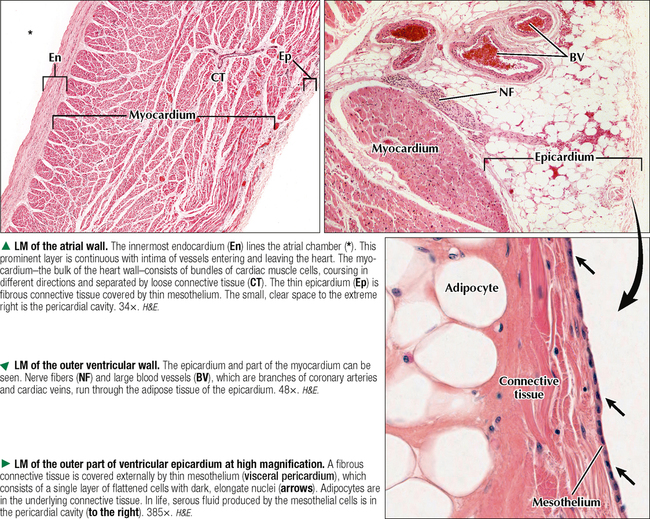
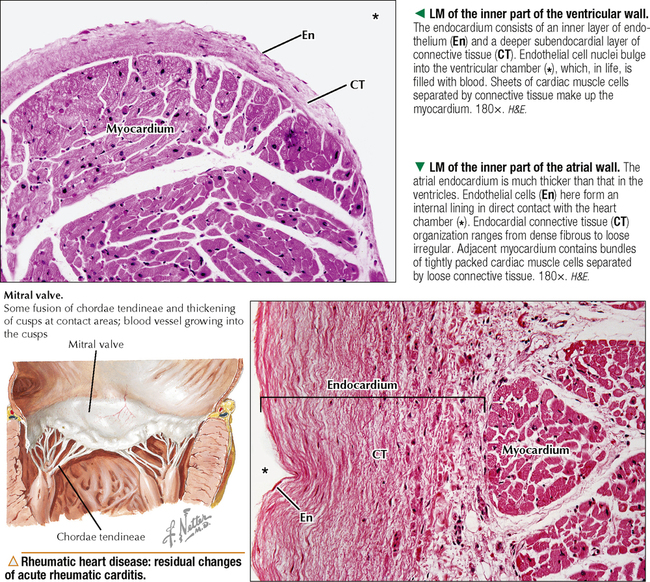
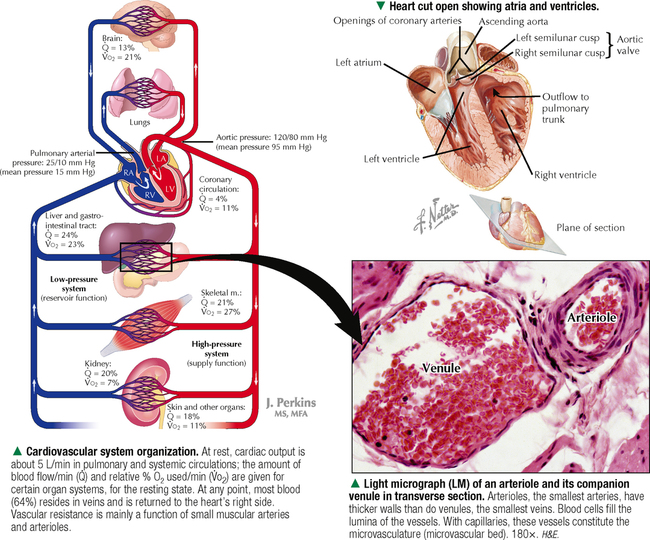
8 The endocardium contains several distinct layers, which may vary histologically in different parts of the heart. An innermost endothelium, derived embryonically from mesoderm, is made of one layer of endothelial cells, which are a type of simple squamous epithelium. It is continuous with endothelium of veins and arteries that enter and leave the heart. A subendothelial layer of connective tissue consists of collagen fibers, elastic fibers, and scattered smooth muscle cells. In some areas is another layer of loose fibroelastic connective tissue, the subendocardium. It may contain elements of the cardiac conduction system, such as Purkinje fibers, which are modified cardiac muscle cells (see Chapter 4). The endocardium is usually thicker in the atria than in the ventricles. The inner surface of the ventricles under the endocardium has trabeculae that project into the lumen and are composed of cardiac muscle—called papillary muscles. Although the luminal surface of the atria is relatively smooth, a small auricular appendage is trabeculated internally by muscular bands, or pectinate muscles. The much thicker ventricular myocardium compared with the atrial layer reflects differences in workload of heart chambers. The myocardium consists of interlacing bundles, or sheets, of cardiac muscle cells embedded in richly vascularized, loose connective tissue, which is the endomysium. The muscle fibers in each sheet have a complex spiral pattern that winds around the atria and ventricles. Cardiac muscle cells form a three-dimensional anastomosing network whereby intercalated discs link almost all cells and other cells insert into the cardiac skeleton of dense fibrous connective tissue.
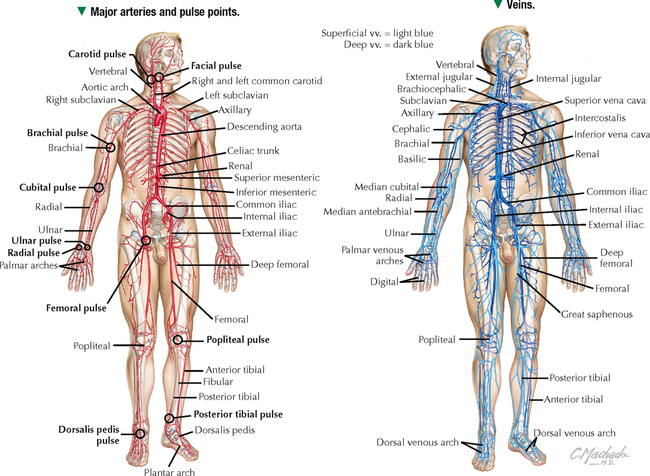
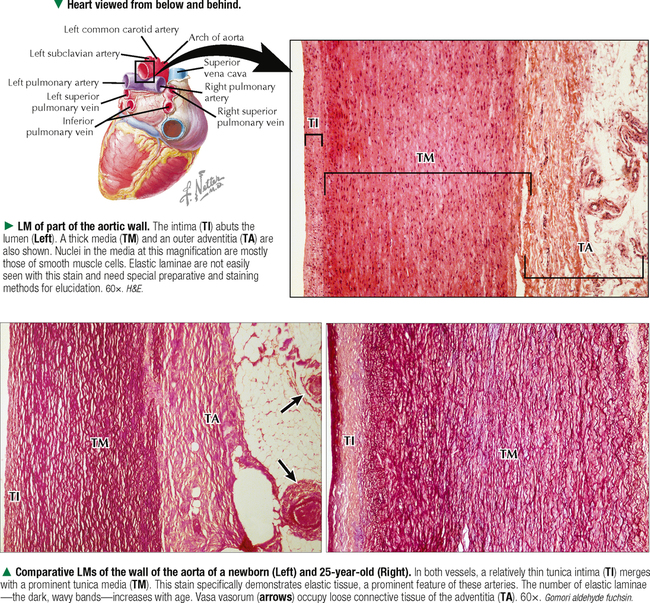
CARDIOVASCULAR SYSTEM
8.3 HISTOLOGY OF THE ENDOCARDIUM AND MYOCARDIUM

Basicmedical Key
Fastest Basicmedical Insight Engine