TERMS
•Adolescence
•Body surface area
•Childhood
•Infant
•Neonate
OBJECTIVES
Upon completion of this chapter, the technician student will be able to:
•Convert pounds to kilograms.
•Convert kilograms to pounds.
•Calculate doses based on milligrams per kilogram and micrograms per kilogram of body weight.
•Determine the body surface area of patients using the West nomogram.
•Calculate doses based on body surface area.
This chapter focuses on dosage calculations relevant to the dispensing of prefabricated dosage forms for the pediatric patient. The methods of determining these dosages are also relevant to adults, the elderly, and others with special needs, such as the chemotherapy patient.
 Pediatric Patients
Pediatric Patients
Pediatrics is the branch of medicine that deals with disease in children from birth through adolescence. Because of the range in age and bodily development in this population, the inclusive groups are defined further as follows: neonate (newborn), aged birth to 1 month; infant, 1 month to 1 year; early childhood, 1 to 5 years; late childhood, 6 to 12 years; and adolescence, 13 to 17 years of age.1
neonate Infant from birth to 1 month of age.
infant A baby aged 1 month to 1 year.
adolescence ages 13 to 17.
Proper dosing of the pediatric patient depends on a number of factors, including the patient’s age and weight, overall health status, the condition of such biologic functions as respiration and circulation, and the stage of development of body systems for drug metabolism (e.g., liver enzymes) and drug elimination (e.g., renal system). In the neonate, these biologic functions and systems are underdeveloped. Renal function, for example, develops over the first 2 years of life. This fact is particularly important because the most commonly used drugs in neonates, infants, and young children are antimicrobial agents, which are eliminated primarily through the kidney. If the rate of drug elimination is not properly considered, drug can accumulate in the body and lead to overdose and toxicity.
Body weight is an important factor used to calculate doses for pediatric patients as well as adults. Two methods are used for calculating safe pediatric doses. Based on body weight, they are calculations of milligrams per kilogram or micrograms per kilogram or according to body surface area (BSA) in square meters. The BSA method is the more accurate and therefore used widely for chemotherapeutic agents. The milligrams per kilogram method is the most frequently used elsewhere. Medications dosed in small amounts may be dosed as micrograms per kilogram.
body surface area A mathematical approximation using the height and weight of a patient and expressing the area of the patient in square meters. The best-known BSA chart is the West nomogram, which can be used for both children and adults.
Over-the-counter medications include labeling instructions that provide guidelines for safe and effective dosing. For pediatric use, doses generally are based on age ranges, e.g., 2 to 6 years old, 6 to 12 years old, and older than 12 years. For children 2 years of age or younger, the label recommendation generally states, “consult your physician.”
In the past, formula methods of pediatric doses were used, some based on age (Young’s, Cowling’s, and Fried’s rules) and one on weight (Clark’s rule). These formulas are not commonly used in today’s practices and need not be memorized by the technician student:
Young’s rule, based on age:
![]()
Cowling’s rule:
![]()
![]()
Clark’s rule, based on weight:
![]()
Oral and parenteral dosages for pediatric patients are often much smaller than those for an adult. Oral doses are often measured in milliliters, sometimes part of a milliliter, and require that the patient’s caregiver be given an accurate measuring device, such as an oral syringe (Fig. 7.1). Parenteral doses may be in tenths or hundredths of a milliliter. Chapter 4 gives examples of measuring devices that caregivers should receive with certain pediatric dosage forms.

Figure 7.1 Two oral syringes, one clear and one amber-colored to protect the medication from light. The amber syringe is calibrated in 0.2-mL increments and marked in half-teaspoonfuls up to 2 tsp.
 Drug Dosage Based on Body Weight
Drug Dosage Based on Body Weight
For calculations of doses based on milligrams per kilogram of body weight it is important to express the child’s weight in kilograms. It is important to memorize the conversion of pounds to kilograms:
1kg = 2.2 lb
Medications based on milligrams per kilogram of body weight are most often milligrams per kilogram per day, sometimes micrograms per kilogram per day. Therefore, to determine a single dose it is necessary to divide the daily dose by the number of doses that will be given a day.
Rules for Calculating Pediatric Doses

1.Convert weight to kilograms.
2.Determine daily dose using rules set forth in Chapter 6:
a.Convert: Be sure all measurements are in the same system and all units are in the same size. Remember to convert to the system of measurement of the drug on hand.
b.Estimate a reasonable amount that should be given.
c.Calculate dose (using ratio-proportion or alternate method).
3.Determine a single dose by dividing the daily dose by the number of doses per day.
4.Determine the quantity of available drug to give. Use the same rules of thumb:
a.Convert
b.Estimate
c.Calculate dose (using ratio-proportion or alternate method)
Critical Thinking 7.1

A prescription was called in to the pharmacy for Cefzil® oral suspension. The order was for 125 mg of Cefzil® suspension every 12 hours for 10 days. The weight of the child was found to be 37 pounds. Upon checking the recommended dose, the pharmacy found the recommendation to be 7.5 mg/kg every 12 hours for 10 days for a pediatric patient. The recommendation for this patient would be 277 mg every 12 hours. The formula the pharmacy used to check the dose was
![]()
What mistakes did the technician make?
What is the recommended dose for the 37-pound child?
Review Set 7.1: Drug Dosage Based on Body Weight
1.Convert pounds to kilograms (round to two decimal places).
a.12 lb
b.20 lb
c.45 lb
d.62 lb
e.7 lb 8 oz
f.4 lb 2 oz
g.2 lb 10 oz
2.Convert kilograms to pounds.
a.12 kg
b.8 kg
c.24 kg
d.70.5 kg
e.35.6 kg
3.Calculate the daily dose in milligrams of the following:
a.250 mg q8h
b.375 mg q12h
c.325 mg q6h
d.750 mcg BID
e.60 mg TID
4.Calculate the single dose in milligrams of the following:
a.750 mg per day in 3 divided doses
b.1 g per day in 4 divided doses
c.500 mg per day q 8h
d.250 mg per day BID
5.Decadron® is recommended at a dose of 0.5 mg/kg per day. If the patient weighs 65 kg, what is the daily dose?
6.A neonatal patient is to receive 6 mL/kg of a drug. How much should a patient who weighs 1.6 kg receive?
7.The recommended dose for drug A is 5 mg/kg q 8h. The patient weighs 22 lb.
a.Calculate a single dose for drug A.
b.Calculate the daily dose for drug A.
c.Drug A is available at 125 mg/5 mL. Calculate the amount to be given for a single dose.
d.Calculate the amount needed to be dispensed for a 10-day supply of drug A.
8.Phenobarbital has a recommended dose of 3.5 mg/kg per day q 12h for maintenance therapy. A child weighing 12 lb was ordered 10 mg q 12h. Is the dose ordered appropriate for this patient?
9.The recommended dosing for cephalexin is 25 to 50 mg/kg per day in four divided doses.
a.What should the dosage range be for a 40-lb child?
b.The order reads, “Cephalexin 125/5, 1½ tsp q 6h.” Is the amount ordered within the recommended guidelines?
10.The dose of gentamicin for premature and full-term neonates is 2.5 mg/kg administered every 12 hours. What is the daily dose for a newborn weighing 5.6 lb?
11.The dose of a drug is 500 mcg/kg of body weight. How much (in milligrams) should be given to a child weighing 55 lb?
12.Using the prescription below, calculate the number of tablets to dispense to a patient weighing 147 pounds.
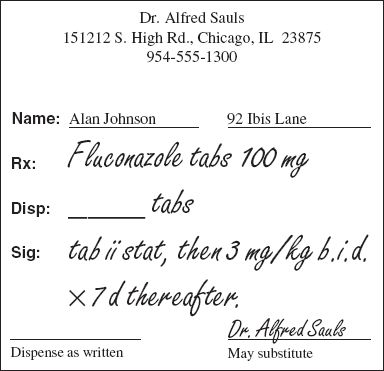
13.If the pediatric dose of dactinomycin is 15 mcg/kg per day for 5 days, how much (in micrograms) should be administered to a 40-lb child over the course of treatment?
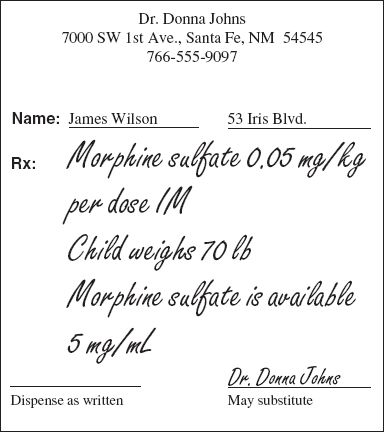
14.Based on the prescription below
a.Calculate a single dose.
b.Calculate the amount in milliliters to give.
15.Amoxicillin is recommended at 20 to 40 mg/kg per day in 3 divided doses. A 44-lb child has an order that reads as follows:
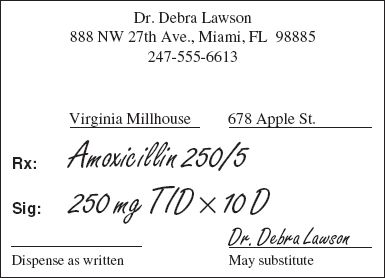
a.Does the order fall within the recommended dosage range?
b.If no, how should the dose be adjusted?
c.If yes, how much should be dispensed to complete the course of therapy?
d.If your answer to part a was no, how much of the readjusted dose you figured out in part b will you dispense to complete the course of therapy?
16.Augmentin® is recommended based on the amoxicillin component. For infants and neonates the recommendation is 30 mg/kg per day every 12 hours. The patient weighs 8 lb. The order reads as follows:
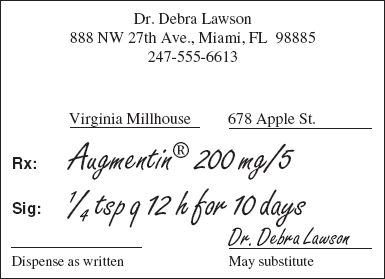
a.Does the order fall within the recommended dose?
b.If no, how should the dose be adjusted?
c.If yes, how much should be dispensed to complete the course of therapy?
d.If your answer to part b was no, how much of the readjusted dose will you dispense to complete the course of therapy?
17.In a neonatal intensive care unit, a 7.4-mg loading dose of aminophylline was ordered for a premature infant. Instead, by a fatal error, 7.4 mL of a 250 mg/10-mL solution was administered.2 How much aminophylline (in milligrams) was administered rather than the prescribed amount?
18.The maintenance dose of Choledyl® is 13.2 mg/kg per day or 800 mg, whichever is less, four times daily. How many 100-mg tablets of the drug should a 200-lb patient take at each dosing interval?
19.A medication order calls for 6 μg/kg of body weight of pentagastrin to be administered subcutaneously to a patient weighing 154 lb. The source of the drug is an ampul containing 0.5 mg in each 2 mL. How many milliliters of the solution should be injected?
20.If the loading dose of kanamycin is 7 mg/kg of body weight, how much (in grams) should be administered to a patient weighing 165 lb?



