http://evolve.elsevier.com/Edmunds/NP/
Calcium channel blockers (CCBs) are indicated for a variety of cardiovascular conditions and are categorized into three subclasses. Only one class, the dihydropyridines, includes more than one commercially available drug. The main difference between the dihydropyridines and the other classes is that the dihydropyridines do not affect the cardiac conduction system. Diltiazem is generally considered to have effects that are more similar to those of verapamil than to those of nifedipine. All drugs in this class are available in generic formulation.
The warning applies only to short-acting nifedipine. Recent studies have shown that CCBs are safe for the long-term treatment of stable symptomatic angina. However, nifedipine did not provide additional protection against new cardiovascular events in patients who were already being treated for angina, hypertension, or hyperlipidemia with effective medications. CCBs are recommended for use when they are necessary to control angina or hypertension in patients who already are receiving proven cardioprotective medications.
Therapeutic Overview
For an overview of hypertension, angina, and arrhythmias see Chapters 17, 18, and 23, respectively.
Mechanism of Action
Although these compounds have diverse chemical structures, they all share a basic electrophysiologic property: they block the inward movement of calcium through the slow channels of the cell membranes of cardiac and smooth muscle cells. The drugs differ in their location of action (Tables 21-2 and 21-3). The three types of tissue cells acted on are as follows:
TABLE 21-3
Effect of Calcium Channel Blockers on Myocardium
++ Moderate increase; + some increase; +- little increase; 0, no effect; – some decrease; — moderate decrease; —pronounced decrease.
Cardiac Muscle
CCBs decrease the force of myocardial contraction by blocking the inward flow of calcium ions through the slow channels of the cell membrane during phase 2 (plateau phase) of the action potential. The diminished entry of calcium ions into the cells thereby fails to trigger the release of large amounts of calcium from the sarcoplasmic reticulum within the cell. This free calcium is needed for excitation-contraction coupling, an event that activates contraction by allowing cross-bridges to form between the actin and myosin filaments of muscle. The number of actin and myosin cross-bridges formed within the sarcomere determines the force of the heart’s contraction. Decreasing the amount of calcium ions released from the sarcoplasmic reticulum causes fewer actin and myosin cross-bridges to be formed, thus decreasing the force of contraction and resulting in a negative inotropic effect. This decreases cardiac output.
Cardiac Conduction System (SA and AV Nodes)
In these tissues, CCBs decrease automaticity in the SA node and decrease conduction in the AV node. Automaticity means that a cell depolarizes spontaneously and initiates an action potential without an external stimulus. Automaticity is a normal characteristic of SA nodal cells. Depolarization (Phase 0) of the action potential is normally generated by the inward calcium ion current through slow channels. Thus, agents that can block the inward calcium ion current across the cell membrane of SA nodal tissue decrease the rate of depolarization and depress automaticity. The result is a variable decrease in heart rate (a negative chronotropic effect) (Figure 21-1). Similarly, an agent that decreases calcium ion influx across the cell membrane of the AV node slows AV nodal conduction (negative chronotropic effect) and prolongs AV refractory time. When AV conduction is prolonged, fewer atrial impulses reach the ventricles, thus slowing the rate of ventricular contractions.
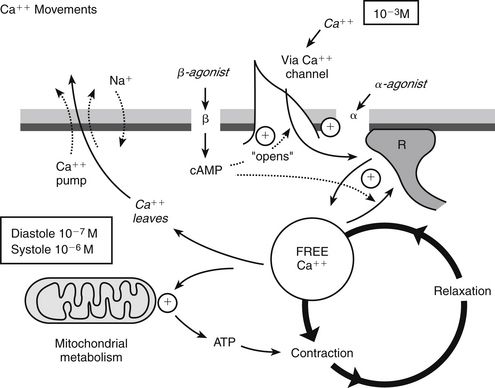
FIGURE 21-1 Physiologic activity of calcium channel blockers. Data from Burton L et al, eds: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11, New York, 2005, McGraw-Hill; National Institutes of Health: The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH Publication No. 03-5233, Washington, DC, 2003, U.S. Government Printing Office.
Vascular Smooth Muscle
The smooth muscle of the coronary and peripheral vessels has a significant influence on afterload and the hemodynamics of circulation. The decreased force of smooth muscle contraction results in coronary artery dilation, which lowers coronary resistance and improves blood flow through collateral vessels, as well as oxygen delivery to ischemic areas of the heart. CCBs dilate the main coronary arteries and arterioles in both normal and ischemic regions. Therefore, drugs with these actions are helpful in the treatment of angina pectoris.
CCBs reduce arterial pressure at rest and at given levels of exercise by dilating peripheral arterioles and reducing the total peripheral resistance (afterload) against which the heart works, resulting in reduced blood pressure. This unloading of the heart reduces myocardial energy consumption and oxygen requirements and probably accounts for the effectiveness of CCBs in chronic stable angina and causes a decrease in blood pressure.
CCBs are potent inhibitors of coronary artery spasm. This property increases myocardial oxygen delivery in patients with coronary artery spasm and is responsible for the effectiveness of CCBs in vasospastic angina.
Specific Calcium Channel Blockers
For an overview of the differences between the subclasses of CCBs, see Table 21-2.
Nifedipine is a potent dilator of vascular smooth muscle that causes decreased peripheral vascular resistance in both coronary arteries and peripheral arterioles. Nifedipine has a mild negative inotropic effect—less than that of verapamil. Usually, a small increase in heart rate occurs, along with a reflex response to vasodilation. Nifedipine has no tendency to prolong AV conduction, prolong SA node recovery time, or slow sinus rate.
Verapamil also dilates vascular smooth muscle, although it is less potent than nifedipine. Verapamil has a significant negative inotropic effect that prevents and blocks reflex tachycardia and relieves coronary artery spasm. This negative inotropic effect decreases myocardial oxygen demand and thus helps to relieve angina-related ischemia and pain. Verapamil also slows conduction in the SA and AV nodes, although it has a greater effect on the AV node.
Diltiazem has a less negative inotropic effect than verapamil and causes less peripheral vasodilation than nifedipine. Diltiazem selectively has more effect on cardiac muscle than on peripheral vascular smooth muscle. It slows conduction through the SA/AV nodes, but not to the extent that verapamil does.
Treatment Principles
For information on standardized treatment guidelines, for evidence supporting these guidelines, and for information on nonpharmacologic treatment for hypertension, angina, and arrhythmia, see the related chapters—Chapters 17, 18, and 23. In this chapter, only pharmacologic treatment with CCBs is discussed.
Arrhythmias
The dihydropyridines—nifedipine and its relatives—are used differently from verapamil and diltiazem, which are similar to each other.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Key drug.
Key drug.
 Short-acting nifedipine should not be used for the acute reduction of blood pressure, the control of essential hypertension, immediately after MI, or in acute coronary artery syndrome.
Short-acting nifedipine should not be used for the acute reduction of blood pressure, the control of essential hypertension, immediately after MI, or in acute coronary artery syndrome.