2-selective agonists, muscarinic antagonists, methylxanthines, and leukotriene receptor blockers. Anti-inflammatory drugs used in asthma include corticosteroids, mast cell stabilizers, and an anti-IgE antibody. Leukotriene antagonists play a dual role.

High-Yield Terms to Learn
Bronchial hyperreactivity Pathologic increase in the bronchoconstrictor response to antigens and irritants; caused by bronchial inflammation IgE-mediated disease Disease caused by excessive or misdirected immune response mediated by IgE antibodies. Example: asthma Mast cell degranulation Exocytosis of granules from mast cells with release of mediators of inflammation and bronchoconstriction Phosphodiesterase (PDE) Family of enzymes that degrade cyclic nucleotides to nucleotides, for example, cAMP (active) to AMP (inactive); various isoforms, some degrade cGMP to GMP Tachyphylaxis Rapid loss of responsiveness to a stimulus (eg, a drug)
Pathophysiology of Asthma
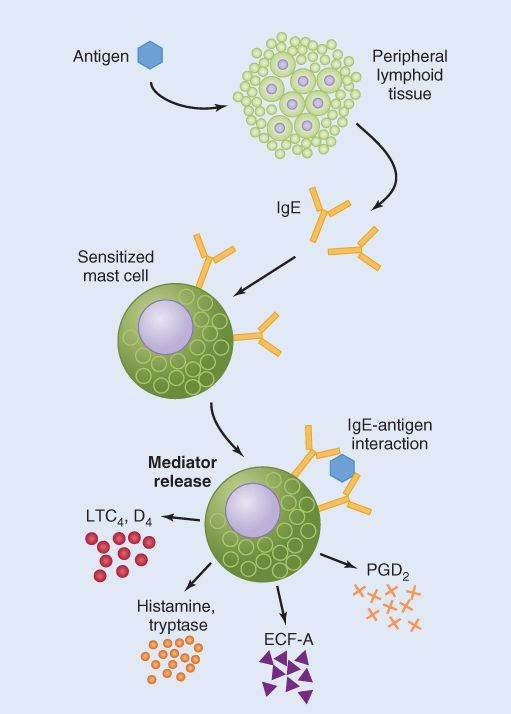
The immediate cause of asthmatic bronchoconstriction is the release of several mediators from IgE-sensitized mast cells and other cells involved in immunologic responses (Figure 20-1). These mediators include the leukotrienes LTC4 and LTD4. In addition, chemotactic mediators such as LTB4 attract inflammatory cells to the airways. Finally, several cytokines and some enzymes are released, leading to chronic inflammation. Chronic inflammation leads to marked bronchial hyperreactivity to various inhaled substances, including antigens, histamine, muscarinic agonists, and irritants such as sulfur dioxide (SO2) and cold air. This reactivity is partially mediated by vagal reflexes.
FIGURE 20-1
Immunologic model for the pathogenesis of asthma. Exposure to antigen causes synthesis of IgE, which binds to and sensitizes mast cells and other inflammatory cells. When such sensitized cells are challenged with antigen, a variety of mediators are released that can account for most of the signs of the early bronchoconstrictor response in asthma. LTC4, D4, leukotrienes C4 and D4; ECF-A, eosinophil chemotactic factor-A; PGD2, prostaglandin D2.
(Modified and reproduced, with permission, from Gold WW: Cholinergic pharmacology in asthma. In: Asthma Physiology, Immunopharmacology, and Treatment. Austen KF, Lichtenstein LM, editors. Academic Press, 1974.)
Strategies of Asthma Therapy
Acute asthmatic bronchospasm must be treated promptly and effectively with bronchodilators (“reliever” drugs). Beta 2 agonists, muscarinic antagonists, and theophylline and its derivatives are available for this indication. Long-term preventive treatment requires control of the inflammatory process in the airways (“controller” drugs). The most important anti-inflammatory drugs in the treatment of chronic asthma are the corticosteroids and drugs (such as cromolyn and nedocromil ) that inhibit release of mediators from mast cells and other inflammatory cells. Long-acting  2 agonists can improve the response to corticosteroids. Anti-IgE antibodies also appear promising for chronic therapy. The leukotriene antagonists have effects on both bronchoconstriction and inflammation but are used only for prophylaxis.
2 agonists can improve the response to corticosteroids. Anti-IgE antibodies also appear promising for chronic therapy. The leukotriene antagonists have effects on both bronchoconstriction and inflammation but are used only for prophylaxis.
Beta-Adrenoceptor Agonists
Prototypes and Pharmacokinetics
The most important sympathomimetics used to reverse asthmatic bronchoconstriction are the  2-selective agonists, although epinephrine and isoproterenol are still available and used occasionally (see Chapter 9). Of the indirect-acting sympathomimetics, ephedrine was once used, but it is now obsolete for this application. Of the selective agents, albuterol, terbutaline, and metaproterenol * are short-acting and are the most important in the United States. Salmeterol and formoterol are long-acting
2-selective agonists, although epinephrine and isoproterenol are still available and used occasionally (see Chapter 9). Of the indirect-acting sympathomimetics, ephedrine was once used, but it is now obsolete for this application. Of the selective agents, albuterol, terbutaline, and metaproterenol * are short-acting and are the most important in the United States. Salmeterol and formoterol are long-acting  2-selective agonists. Beta agonists are given almost exclusively by inhalation, usually from pressurized aerosol canisters but occasionally by nebulizer. The inhalational route decreases the systemic dose (and adverse effects) while delivering an effective dose locally to the airway smooth muscle. The older drugs have durations of action of 6 h or less; salmeterol and formoterol act for 12 h or more.
2-selective agonists. Beta agonists are given almost exclusively by inhalation, usually from pressurized aerosol canisters but occasionally by nebulizer. The inhalational route decreases the systemic dose (and adverse effects) while delivering an effective dose locally to the airway smooth muscle. The older drugs have durations of action of 6 h or less; salmeterol and formoterol act for 12 h or more.
*Do not confuse metaproterenol, a  2 agonist, with metoprolol, a
2 agonist, with metoprolol, a  -blocker.
-blocker.
Mechanism and Effects
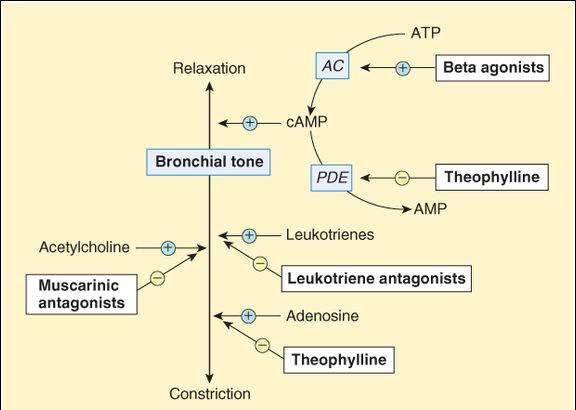
Beta-adrenoceptor agonists stimulate adenylyl cyclase (via the  2-adrenoceptor-Gs-coupling protein-adenylyl cyclase pathway) and increase cyclic adenosine monophosphate (cAMP) in smooth muscle cells (Figure 20-2). The increase in cAMP results in a powerful bronchodilator response.
2-adrenoceptor-Gs-coupling protein-adenylyl cyclase pathway) and increase cyclic adenosine monophosphate (cAMP) in smooth muscle cells (Figure 20-2). The increase in cAMP results in a powerful bronchodilator response.
FIGURE 20-2
Possible mechanisms of  agonists, muscarinic antagonists, theophylline, and leukotriene antagonists in altering bronchial tone in asthma. AC, adenylyl cyclase; PDE, phosphodiesterase.
agonists, muscarinic antagonists, theophylline, and leukotriene antagonists in altering bronchial tone in asthma. AC, adenylyl cyclase; PDE, phosphodiesterase.
Clinical Use
Sympathomimetics are first-line therapy in acute asthma. Shorter acting sympathomimetics (albuterol, metaproterenol, terbutaline) are the drugs of choice for acute episodes of bronchospasm. Their effects last for 4 h or less, and they are not effective for prophylaxis. The long-acting agents (salmeterol, formoterol) should be used for prophylaxis, in which their 12-h duration of action is useful. They should not be used for acute episodes because their onset of action is too slow. Furthermore, used alone, they increase asthma mortality, whereas in combination with corticosteroids, they improve control. In almost all patients, the shorter-acting  agonists are the most effective bronchodilators available and are life-saving for acute asthma. Many patients with chronic obstructive pulmonary disease (COPD) also benefit, although the risk of toxicity is increased in this condition.
agonists are the most effective bronchodilators available and are life-saving for acute asthma. Many patients with chronic obstructive pulmonary disease (COPD) also benefit, although the risk of toxicity is increased in this condition.
Toxicity
Skeletal muscle tremor is a common adverse  2 effect. Beta2 selectivity is relative. At high clinical dosage, these agents have significant
2 effect. Beta2 selectivity is relative. At high clinical dosage, these agents have significant  1 effects. Even when they are given by inhalation, some cardiac effect (tachycardia) is common. Other adverse effects are rare. When the agents are used excessively, arrhythmias may occur. Loss of responsiveness (tolerance, tachyphylaxis) is an unwanted effect of excessive use of the short-acting sympathomimetics. Patients with COPD often have concurrent cardiac disease and may have arrhythmias even at normal dosage.
1 effects. Even when they are given by inhalation, some cardiac effect (tachycardia) is common. Other adverse effects are rare. When the agents are used excessively, arrhythmias may occur. Loss of responsiveness (tolerance, tachyphylaxis) is an unwanted effect of excessive use of the short-acting sympathomimetics. Patients with COPD often have concurrent cardiac disease and may have arrhythmias even at normal dosage.
Methylxanthines
Prototypes and Pharmacokinetics
The methylxanthines are purine derivatives. Three major methylxanthines are found in plants and provide the stimulant effects of 3 common beverages: caffeine (in coffee), theophylline (tea), and theobromine (cocoa). Theophylline is the only member of this group that is important in the treatment of asthma. The drug and several analogs are orally active and available as various salts and as the base. Theophylline is available in both prompt-release and slow-release forms. Theophylline is eliminated by P450 drug-metabolizing enzymes in the liver. Clearance varies with age (highest in young adolescents), smoking status (higher in smokers), and concurrent use of other drugs that inhibit or induce hepatic enzymes.
Mechanism of Action
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree