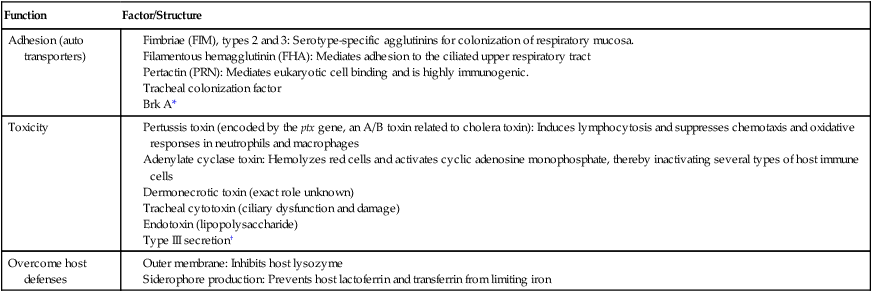
1. Describe the general characteristics of the Bordetella spp. 2. State the normal habitat and routes of transmission for Bordetella pertussis and Bordetella parapertussis. 3. Describe the three stages of pertussis, including the duration and symptoms. 4. Describe the proper collection and transport of specimens for the detection of B. pertussis and B. parapertussis. 5. Explain the limitations of direct fluorescent antibody (DFA) and polymerase chain reaction (PCR) methods for detecting B. pertussis, including assay specificity and sensitivity. 6. Describe the optimum condition for culturing B. pertussis, including specimens of choice for optimal recovery. 7. Outline the major tests used to identify and differentiate B. pertussis and B. parapertussis. 8. Correlate the patient’s signs and symptoms and laboratory results to identify the etiologic agent associated with infection. The genus Bordetella includes three primary human pathogens: Bordetella bronchiseptica, B. pertussis, and B. parapertussis. B. bronchiseptica is reviewed in Chapter 25 because it grows on MacConkey agar. Although B. parapertussis also can grow on MacConkey agar, it is discussed with B. pertussis in this chapter for two reasons: B. pertussis and B. parapertussis both cause human upper respiratory tract infections, with almost identical symptoms, epidemiology, and therapeutic management; and optimal recovery of both organisms from respiratory specimens requires the addition of blood and/or other suitable factors to culture media. Additional Bordetella species may cause rare asymptomatic infections in immunocompromised patients; these include B. hinzii, B. holmesii, B. petrii, and B. trematum. (See the chapter cross-references in the preceding table for information on organisms not discussed in this chapter.) General features of Bordetella spp. other than B. pertussis and B. parapertussis are summarized in Chapter 25. In contrast to B. bronchiseptica, B. pertussis and B. parapertussis are nonmotile and infect only humans. In the evolutionary process, these exclusive human pathogens have a close genetic relationship. They remain separate species based on their differences in pathogenesis and host range. B. pertussis, the primary pathogen of whooping cough, uses several mechanisms to overcome the immune defenses of healthy individuals. The mechanisms are complex and involve the interplay of several virulence factors (Table 37-1). Some factors help establish infection; others are toxigenic to the host; and still others override specific components of the host’s mucosal defense system. For example, when B. pertussis reaches the host’s respiratory tract, its surface adhesins attach to respiratory ciliated epithelial cells and paralyze the beating cilia by producing a tracheal cytotoxin. A major virulence factor, pertussis toxin (PT), is produced by the attached organism. PT enters the bloodstream, subsequently binding to specific receptors on host cells. After binding, PT disrupts several host cell functions, such as initiation of host cell translation; inability of host cells to receive signals from the environment causes a generalized toxicity. The center membrane of B. pertussis blocks access of the host’s lysozyme to the bacterial cell wall via its outer membrane. B. pertussis and B. parapertussis share a nearly identical virulence control system encoded by the bvgAS locus that is responsive to variation in environmental conditions. Because of this very complex system, Bordetella organisms appear to be able to alter phenotypic expression, enhancing transmission, colonization, and survival. TABLE 37-1 Major Virulence Determinants of Bordetella pertussis *Plays a role in pathogenesis by conferring serum resistance. †This type of secretion allows Bordetella organisms to transport proteins directly into host cells; it is required for persistent tracheal colonization. Several factors influence the clinical manifestations of B. pertussis (Box 37-1). Classic pertussis is usually a disease of children and can be divided into three symptomatic stages: catarrhal, paroxysmal, and convalescent. During the catarrhal stage, symptoms are the same as for a mild cold with a runny nose and mild cough; this stage may last several weeks. Episodes of severe and violent coughing increase in number, marking the beginning of the paroxysmal stage. As many as 15 to 25 paroxysmal coughing episodes can occur in 24 hours; these are associated with vomiting and with “whooping,” the result of air rapidly inspired into the lungs past the swollen glottis. Lymphocytosis occurs, although typically the patient has no fever and no signs and symptoms of systemic illness. This stage may last 1 to 4 weeks. Confirming the diagnosis of pertussis is challenging. Culture, which is most sensitive early in the illness, has been the traditional diagnostic standard for pertussis and shows nearly 100% specificity but varied sensitivity. Organisms may become undetectable by culture 2 weeks after the start of paroxysms. Nasopharyngeal aspirates or a nasopharyngeal swab (calcium-alginate or Dacron on a wire handle) are acceptable specimens, because B. pertussis colonizes the ciliated epithelial cells of upper respiratory tract. Calcium-alginate swabs with aluminum shafts are not recommended for PCR, because they may inhibit the polymerase enzyme in PCR detection. In addition, cotton swabs may be inhibitory to specimen growth and are not recommended. Specimens obtained from the throat, sputum, or anterior nose are unacceptable, because these sites are not lined with ciliated epithelium. For collection, the swab is bent to conform to the nasal passage and held against the posterior aspect of the nasopharynx. If coughing does not occur, another swab is inserted into the other nostril to initiate the cough. The swab is left in place during the entire cough, removed, and immediately inoculated onto a selective medium at the bedside (Table 37-2). TABLE 37-2 Examples of Selective Media for Primary Isolation of B. pertussis and B. parapertussis *Cephalexin is superior to methicillin and penicillin for inhibiting normal respiratory flora. †Regan-Lowe agar has been found to work best for recovery of B. pertussis from nasopharyngeal swabs.
Bordetella pertussis, Bordetella parapertussis, and Related Species
General Characteristics
Epidemiology and Pathogenesis
Epidemiology
Pathogenesis
Spectrum of Disease
Laboratory Diagnosis
Specimen Collection, Transport, and Processing
Agar Media
Description
Bordet-Gengou
Potato infusion agar with glycerol and sheep blood with methicillin or cephalexin* (short shelf-life)
Modified Jones-Kendrick charcoal
Charcoal agar with yeast extract, starch, and 40 µg cephalexin (2- to 3-month shelf-life but inferior to Regan-Lowe agar)
Regan-Lowe†
Charcoal agar with 10% horse blood and cephalexin (4- to 8-week shelf-life)
Stainer-Scholte
Synthetic agar lacking blood products
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
