Blastic Plasmacytoid Dendritic Cell Neoplasm
Aaron Auerbach, MD, PhD
Key Facts
Terminology
Tumor of plasmacytoid dendritic cells, often involves the skin and bone marrow, and disseminates to blood
Clinical Issues
Incidence
Rare
Natural history
Clinically aggressive
Gender/sex
Middle age to elderly, male predominance
Multiple skin lesions
Usually eventually disseminated disease
Prognosis and therapy
Poor response to lymphoma chemotherapy
Therapy for acute lymphoblastic leukemia is most effective
Microscopic Pathology
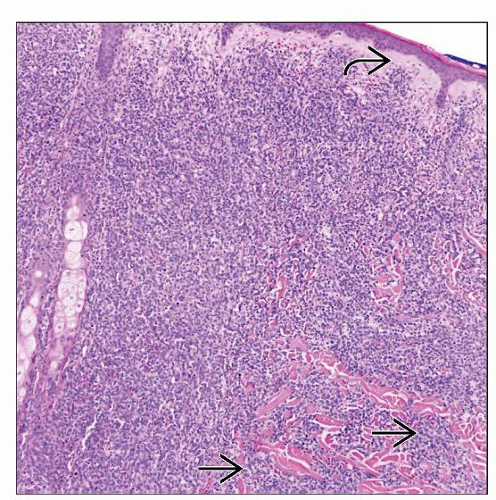
Diffuse dermal infiltrate, spares epidermis, of medium-sized cells with blastic chromatin
Ancillary Tests
Immunohistochemistry: CD123(+), CD4(+), CD56(+), TCL1(+), TdT(+) (sometimes)
Molecular tests
All IgH gene rearrangement studies are nonclonal
Most T-cell receptor gene rearrangement studies are nonclonal
EBV-encoded small nuclear RNA (EBER) negative
Top Differential Diagnoses
Leukemia cutis
Extranodal NK/T-cell lymphoma, nasal type
Peripheral T-cell lymphoma, NOS
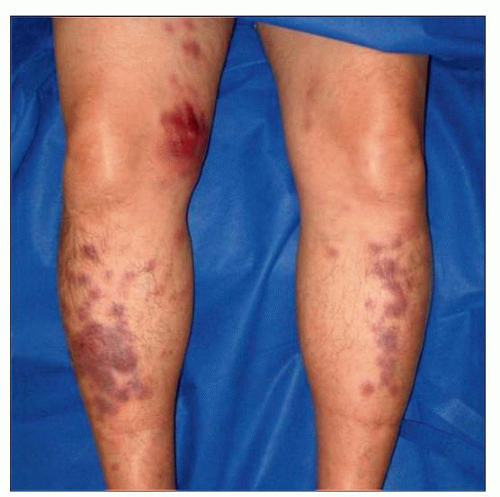 This patient rapidly developed generalized, indurated, purplish-red, well-defined papules and coalescent plaques over his legs. (Courtesy J. Alonso, MD.) |
TERMINOLOGY
Abbreviations
Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
Terminology in 4th edition of World Health Organization classification
Synonyms
CD4(+)/CD56(+) hematodermic neoplasm
CD4(+)/CD56(+) blastic tumor of skin
Blastic NK-cell lymphoma
Agranular CD4(+) natural killer cell leukemia
Definitions
Aggressive tumor of precursor plasmacytoid dendritic cells, which usually involves the skin; frequently culminates in leukemia
Included in the T-cell/NK-cell neoplasm section of the WHO classification, even though it is a tumor of plasmacytoid dendritic cells
ETIOLOGY/PATHOGENESIS
Plasmacytoid Dendritic Cells (PDCs)
PDCs are found in T-cell areas of hematopoietic tissue
Found in lymph node, bone marrow, blood, and spleen (subcapsular)
Enter lymph node and mucosa in response to immune activation
Functions of plasmacytoid dendritic cells
Interferon-γ production
IL-3α expression
Dendritic cell differentiation following exposure to IL3 and CD40
Immunophenotype of plasmacytoid dendritic cells
Positive for
CD4, CD123, BDCA-2, CLA, TCL1, HLA-DR, CD43, CD68
Negative for
CD56, TdT, TIA-1, perforin
Diseases with ↑ plasmacytoid dendritic cells
Castleman lymphadenopathy
Kikuchi-Fujimoto disease
Classic Hodgkin lymphoma
Chronic granulomatous inflammation
Psoriasis
Lupus erythematosus
CLINICAL ISSUES
Epidemiology
Incidence
Rare
< 1% of all acute leukemias
< 1% of cutaneous lymphomas
Age
Usually middle age to elderly
Can occur in children
Median: 65 years
Range: 8-96 years
Gender
M:F = 3.3:1.0
Ethnicity
No association
Site
Often presents in > 1 anatomic site
Skin
Most common 1st manifestation of disease
Eventually skin involvement in nearly all patients
50% confined to skin at initial staging
Bone marrow and peripheral blood
60-90% of cases
There are rare leukemia variants without skin involvement that are recognized with intensive immunophenotyping
Can be subtle infiltrates in bone marrow
Lymph node
45% of cases
Other organs that have been reported to be involved by BPDCN
Liver, spleen, tonsils, nasopharynx, conjunctiva, kidneys, central nervous system
Presentation
Generalized, localized, or solitary cutaneous lesions
Macules, plaques, &/or tumors
Sometimes erythema &/or purpura
Lymphadenopathy
Rarely B symptoms present
Laboratory Tests
Cytopenias
Thrombocytopenia most common
Monocytosis is sometimes present
Natural History
Relapse and metastasis in most cases
Soft tissue and CNS frequently at relapse, but rare at diagnosis
Leukemia
Often relapses as leukemia
10-20% of cases develop into acute myeloid leukemia
Often myelomonocytic leukemia
Presents more like leukemia than lymphoma
Treatment
Adjuvant therapy
Multiagent chemotherapy
Poor response to non-Hodgkin lymphoma chemotherapy (R-CHOP)
90% of cases relapse after chemotherapy
Acute lymphoblastic leukemia protocols
Intrathecal chemotherapy followed by allogeneic bone marrow transplantation
Most effective therapy, especially in children
Prognosis
Poor
Median survival ˜ 13 months
Less aggressive in children with median survival of 3 years
Often favorable initial response to chemotherapy, but eventual relapse
MACROSCOPIC FEATURES
General Features
Nodules, tumors, or plaques of skin, which may have ulceration
MICROSCOPIC PATHOLOGY
Histologic Features
Skin
Dermal infiltrate
Typically extends into subcutaneous tissue
Spares the epidermis with grenz zone
Growth pattern
Diffuse, if extensive involvement
Perivascular
Periadnexal
Increased mitotic figures
Extravasated erythrocytes
Scattered reactive T cells amidst tumor cells
Lymph node
Effacement of lymph node architecture
Often interfollicular and medullary involvement by tumor
Sometimes tumor in sinuses
Bone marrow
Aggregates of tumor cells or scattered tumor cells
Often interstitial distribution
Residual bone marrow often shows dysplasia
Peripheral blood
Tumor cells can have vacuoles in the cytoplasm
Pseudopods
Resemble monoblasts
ANCILLARY TESTS
Histochemistry
MPO
Reactivity: Negative
Staining pattern
Cytoplasmic
NSE
Reactivity: Negative
Staining pattern
Cytoplasmic
Immunohistochemistry
Plasmacytoid dendritic cell antibodies
CD123(+), BDCA-2/CD303(+)
These are the 2 most specific markers
CD4(+)
May be weakly positive
CD56(+)
May be weakly positive
Rarely CD56 is negative, and does not exclude the diagnosis
TCL1(+)
Also positive in some lymphomas, but negative in AML
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree