Blastic Plasmacytoid Dendritic Cell Neoplasm
Wesley O. Greaves, MD
L. Jeffrey Medeiros, MD
Key Facts
Clinical Issues
Median age: ˜ 65 years
Wide age range: 8-96 years
Male to female ratio: ˜ 2-3:1
Skin is most common initial site of disease
Other common sites of disease at initial diagnosis
Lymph nodes
Bone marrow and blood
No established standard therapy
Very aggressive clinical course; median survival 12-14 months
Microscopic Pathology
Skin: Diffuse dermal infiltrate
Lymph nodes: Paracortical or diffuse replacement
Bone marrow: Interstitial pattern
Neoplastic cells can exhibit spectrum of findings
Small/intermediate size resembling lymphoblasts
Intermediate size and resembling myeloblasts
Ancillary Tests
Characteristic immunophenotype
CD123(+), TCL1(+), CD303(+), bcl-11A(+)
CD4(+), CD56(+)
TdT expressed in ˜ 50% of cases
CD45/LCA(+), CD99(+/-)
Conventional cytogenetics
Complex karyotype common
Top Differential Diagnoses
Myeloid/monocytic sarcoma or leukemia
T lymphoblastic leukemia/lymphoma
PDC proliferations associated with myeloid neoplasms
TERMINOLOGY
Abbreviations
Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
Current term in 4th edition of World Health Organization (WHO) classification
Synonyms
CD4(+), CD56(+) hematodermic neoplasm/tumor
CD4(+), CD56(+) blastic tumor of skin
Blastic NK-cell lymphoma (3rd edition of WHO classification)
Definitions
Highly aggressive neoplasm derived from precursors of plasmacytoid dendritic cells
ETIOLOGY/PATHOGENESIS
Normal Plasmacytoid Dendritic Cells (PDCs)
Other terms used for PDCs
Type 2 dendritic cells (DC2)
Plasmacytoid monocytes (obsolete)
Plasmacytoid T cells (obsolete)
Mostly located in T-zones of lymphoid tissues
Also present in bone marrow and blood
PDCs are characterized by
High expression of IL-3α chain receptor
Production of interferon-γ
Differentiate into dendritic cells in culture after treatment with IL3 and CD40 ligand
PDCs are increased in a number of diseases including
Lymph nodes
Chronic granulomatous inflammation
Kikuchi-Fujimoto disease, Castleman disease
Classical Hodgkin lymphoma
Skin
Psoriasis
Lupus erythematosus
Immunophenotype of normal PDCs
CD4(+), CD123(+), HLA-DR(+)
CD303/BDCA-2(+), CLA(+), TCL1(+)
GZM-B(+), CD43(+, dim), CD68(+, dim)
CD11c(-), CD56(-), TIA1(-), perforin(-)
Etiology & Pathogenesis of BPDCN Unknown
Associated with myelomonocytic leukemia in ˜ 10-20% of cases
With or without underlying myelodysplasia
CLINICAL ISSUES
Epidemiology
Incidence
Rare
< 1% of all lymphomas that involve skin
Age
Median age: ˜ 65 years
Wide age range: 8-96 years
Gender
Male to female ratio: ˜ 2-3:1
Ethnicity
No known ethnic predilection
Site
Skin is most common initial site of disease
Other common sites of disease at time of initial diagnosis
Lymph nodes
Bone marrow and blood
Usually low-level involvement
Staging studies can show involvement of
Spleen, liver, other viscera
Other rare sites of disease
Tonsils, nasopharynx, gums
Lacrimal gland, conjunctiva
Kidneys, gynecologic tract
Central nervous system involvement is rare at diagnosis
Involved in ˜ 33% of patients at time of relapse
Mediastinum is rarely involved
Presentation
Solitary or multiple skin lesions
Nodules, patch-like, or plaques
± erythema, ± purpura
Can be asymptomatic
Disease restricted to skin in ˜ 50% of patients
Regional lymph nodes positive in ˜ 50% of patients
Low-level blood and bone marrow involvement
Systemic B symptoms are uncommon
Laboratory Tests
Complete blood count
± cytopenias
± monocytosis
BPDCN can progress to full-blown leukemic phase
Neoplastic cells may be either BPDCN or myelomonocytic leukemia
Treatment
No established standard therapy; options usually employed
Combination chemotherapy
Allogeneic stem cell transplantation at first relapse
Localized radiotherapy has limited utility
Prognosis
Very aggressive clinical course
Median survival: 12-14 months
Patients often have good initial response to chemotherapy
Relapse and disease progression very common
Skin lesions respond to radiotherapy, but this modality has limited utility
Few patients enter long-term remission after stem cell transplantation
Prognosis is relatively better for patients < 40 years
Median survival: ˜ 3 years
IMAGE FINDINGS
Radiographic Findings
Increased uptake by [18F] fluorodeoxyglucose positron emission tomography
MACROSCOPIC FEATURES
General Features
Nodules, plaques, or bruise-like lesions of skin
± ulcer
MICROSCOPIC PATHOLOGY
Histologic Features
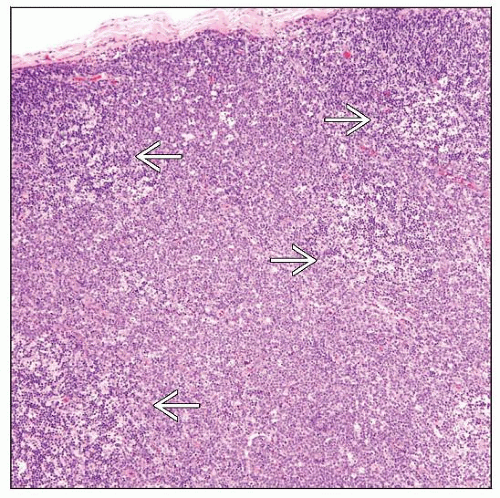
Skin
Monomorphous infiltrate predominantly involving dermis
Perivascular and periadnexal pattern in lesions with minimal involvement
Diffuse pattern with extensive involvement
Grenz zone usually present between infiltrate and epidermis
No or minimal epidermotropism
Erythrocyte extravasation is common
Modest inflammatory infiltrate associated with neoplasm
Small number of T cells
Usually no plasma cells or eosinophils
Lymph node
Diffuse effacement of lymph node architecture
In cases with partial involvement
Preferential paracortical replacement
Sinuses can be involved
Bone marrow
Mild to marked interstitial infiltration
Dysplasia in residual hematopoietic cells
Can be prominent in megakaryocytes
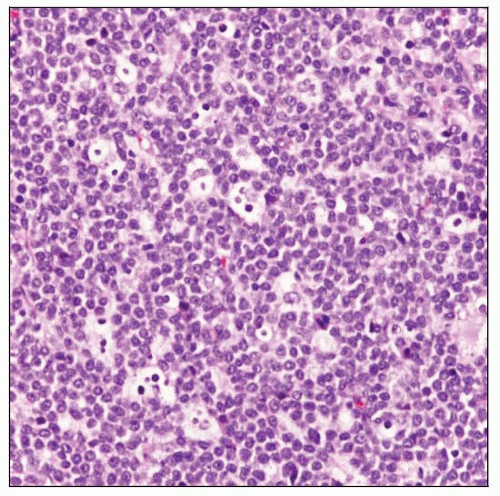
Cytologic Features
Neoplastic cells can exhibit spectrum of findings
Small to intermediate size and resembling lymphoblasts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree