23 Birth Outcomes
A Global Perspective
I Birth Counts
The estimated 135 million babies born worldwide1 enter very different worlds in terms of the care that they and their mothers receive. Also, very different databases are associated with their birth and, if they die, their mortality.
Although celebrated in rich countries, childbirth in many poorer countries is accompanied by apprehension for the mother and newborn, who may remain hidden at home with limited access to care. More than 98% of neonatal mortality (death in first 28 days after birth)2 and third-trimester stillbirths (death of fetus in utero at ≥1000 g birth weight or ≥28 completed weeks’ gestation)3 occur in low-income and middle-income countries, and approximately half occur at home. In poor communities, many babies die unnamed and unrecorded, the majority of these without record of birth or death.4,5 Often the live-born baby is unnamed until several weeks have passed, reflecting a sense of fatalism and perceived inevitability of high mortality.4,6
For the 60 million women giving birth outside a health facility each year, physical distance is often a barrier to care seeking.6 In many cases, cultural norms also keep pregnancy hidden and preclude care seeking outside the home at birth or in the postnatal period, generally considered up to 6 weeks after birth.7 Should complications occur, which may be understood as having a nonbiomedical cause, traditional remedies are often used.8 Although many gaps exist in delivery of services, understanding and addressing the sociocultural context are also critical to accelerating demand and improving coverage of effective care.
In contrast, the 1% of neonatal deaths that occur in rich countries are the subject of confidential inquiries and public outcry if services are considered substandard.9 The majority of published trials of neonatal interventions focus on these relatively few deaths in high-income countries.10,11 The “inverse care law,” first described in Britain in the 1960s, still holds true: the availability of good medical care tends to vary inversely with the need for it in the population served.12 This law could appropriately be extended to the “inverse information and inverse care law”: those communities with the most deaths have the least information on them and the least access to cost-effective interventions to prevent them.4
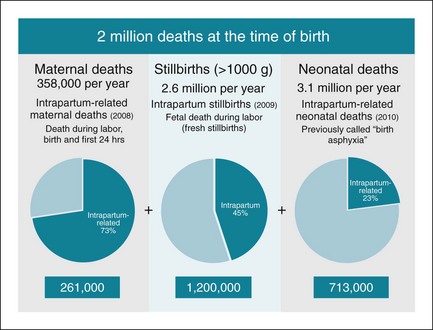
Birth is the time in the human life span with the greatest risk of death. Each year an estimated 720,000 babies die soon after birth from intrapartum-related injury, particularly childbirth complications, primarily in low- and middle-income countries.13 These deaths are closely linked to at least 1.2 million stillbirths occurring during labor.14 In addition, an unknown number of babies survive preterm birth and intrapartum or other insults, only to have long-term impairment and thus are not able to reach their full potential.15 During this same period, the majority of the world’s approximately 300,000 maternal deaths occur, as well as many more “near-miss” maternal deaths and significant maternal morbidity.16–18 Therefore, a total of about 2 million deaths occur at birth, making this a critical time for programmatic focus and emphasizing the need for effective epidemiologic data14,19 (Fig. 23-1).
II Defining Birth Outcomes
A Epidemiologic Definitions and Time Periods
The term perinatal mortality refers to deaths occurring before or soon after birth, including stillbirths and neonatal deaths.20 Historically, there was an advantage in combining these two mortality outcomes, because even in settings with skilled personnel present at birth, significant misclassification occurs between stillbirths and early neonatal deaths.21 However, epidemiologists now prefer that the two specific outcomes of stillbirth and neonatal death are defined and reported as distinct outcomes for a number of reasons.22 First, the combination hides the data issues associated with underreporting between the two outcomes.23 Second, there is inconsistency in the use of the term “perinatal,” which may refer to eight or more different time periods, depending on the definitions used. For example, stillbirths may be defined as fetal deaths occurring at 18, 20, 22, 23, 24, or 28 weeks’ gestation, depending on the definitions used.24,25 The neonatal component may include only “early” neonatal deaths (1-7 days) or “all” neonatal deaths (1-28 days).
The World Health Organization (WHO) International Classification of Diseases (ICD) is widely used as a standard to define conditions and causes of death.26 Figure 23-2 shows the main definitions related to neonatal deaths and stillbirths.
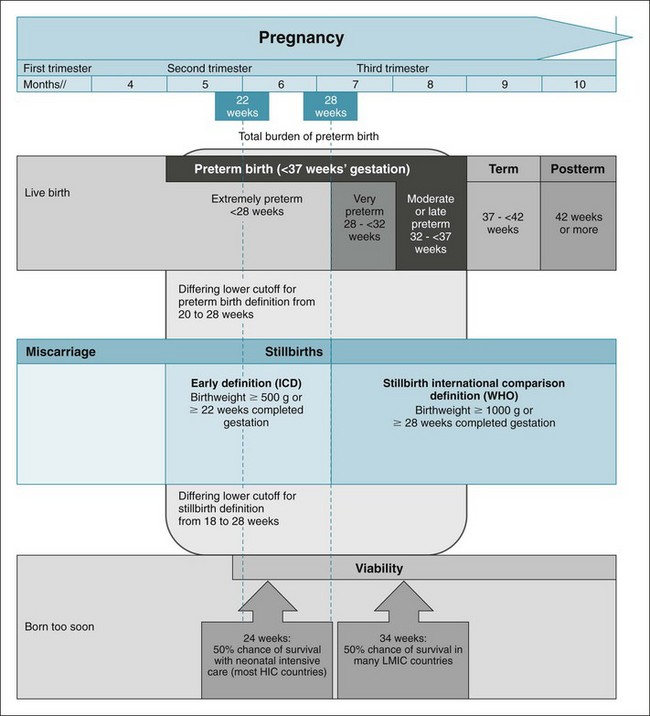
Figure 23-2 Overview of definitions for pregnancy outcomes related to preterm birth and stillbirths.
WHO, World Health Organization; World Bank income groupings: HIC, high-income countries; LMIC, low- and middle-income countries.
(From Blencowe H, Cousens S, Chou D, et al: 15 million preterm births: priorities for action based on national, regional and global estimates. In Howson C, Kinney M, Lawn JE, et al, editors: Born too soon: the global action report on preterm birth. March of Dimes, Partnership for Maternal, Newborn and Child Health, Save the Children, Geneva, 2012 World Health Organization; and www.data.worldbank.org/about/country-classifications/country-and-lending-groups.)
1 Preterm Birth and Stillbirth
Preterm birth is defined by WHO as all births before 37 completed weeks of gestation, or fewer than 259 days since the first day of a woman’s last menstrual period.27 Preterm birth can be further subdivided based on gestational age: extremely preterm (<28 weeks’ gestation), very preterm (28 to <32 weeks), and moderate preterm (32 to <37 completed weeks) (Figure 23-2).25 Moderate preterm birth may be further split to focus on late preterm birth (34 to <37 completed weeks). Recent thinking has questioned this definition, noting that even babies born at 37 or 38 weeks have higher risks than those born at 39 to 41 weeks.28,29
Stillbirth is generally defined as a birth without signs of life (i.e., no breathing, movement, or heart rate after birth).14 The international definition for stillbirth uses stillbirths greater than 1000 g or 28 weeks’ gestation to differentiate stillbirth from miscarriage.3,14 For the stillbirth rate, the denominator includes all births (live births plus stillbirths) using these standard cutoff points, improving the ability to compare rates across countries and over times.3,14 In contrast, for preterm birth, the ICD encourages the inclusion of all live births.26,30 This definition for preterm birth has no lower gestational age or birth weight boundary which complicates the comparison of reported preterm birth rates both between countries and within countries over time, since perceptions of viability of extremely preterm babies change with increasingly sophisticated neonatal intensive care.31 In addition, some reports use nonstandard cutoffs for upper gestational age (e.g., including babies born at up to 38 completed weeks of gestation).30
About 80% of all stillbirths in high-income countries are born preterm, potentially accounting for 5% of all preterm births.9 However, these are excluded from the international preterm birth rates. Thus, counting only live births underestimates the true burden of preterm birth in terms of effect on the health system and on families.
B Real World Definitions
Although it is recommended that all newborns with any signs of life at birth count as live births, for extremely preterm babies, medical practice is variable and associated with perceptions of viability for extremely preterm babies and stillbirth registration thresholds.32,33 In some high-income and middle-income countries, the official definitions of live birth or stillbirth have changed over time. Even without an explicit lower gestational age cutoff in national definitions, the medical care given and whether or not birth and death registration occurs may depend on these perceptions of viability. Therefore, even if no official lower gestational age cutoff is specified for recording a live birth, misclassification of a live birth to “stillbirth” is more common if the medical team perceives the baby to be extremely preterm and thus less likely to survive.31,32
Data quality is particularly affected by underregistration of extremely preterm births or their misclassification to “stillbirths” near the thresholds of perceived viability and variable standards for stillbirth registration.30 Countries using preterm birth definitions that include all births (both stillborn and live-born) from 20 weeks on report a higher proportion of preterm births under 28 weeks (~9%); other countries including live births only consistently report proportions of preterm less than 28 weeks of about 5% (Fig. 23-3).34
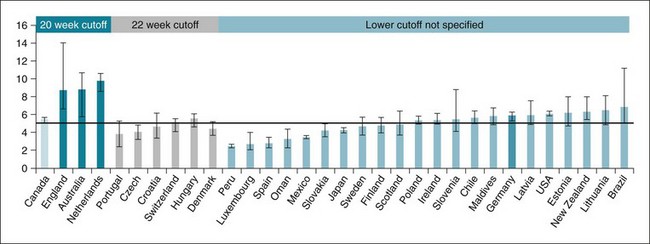
Figure 23-3 Mean percentage of all reported preterm births less than 28 weeks’ gestation by country.
Data from 32 countries with at least one reported data point providing information on the proportion of preterm births that are less than 28 weeks of gestation. Error bars show range of reported proportions. All these countries report using live births as numerator/denominator except for England, Australia, Netherlands, and Germany, who report using total births.
(From Blencowe H, Cousens S, Oestergaard M, et al: National, regional and worldwide estimates of preterm birth rates in the year 2010 with time trends for selected countries since 1990: a systematic analysis and implications. Lancet 379:2162–2172, 2012.)
When thresholds are changed, it may take some time before recording of cases near the new threshold improves. For example, Denmark changed the lower threshold for registering preterm births from 28 to 22 weeks in 1997, but it was 5 years later when the proportion of all preterm births under 28 weeks increased (Fig. 23-4).34
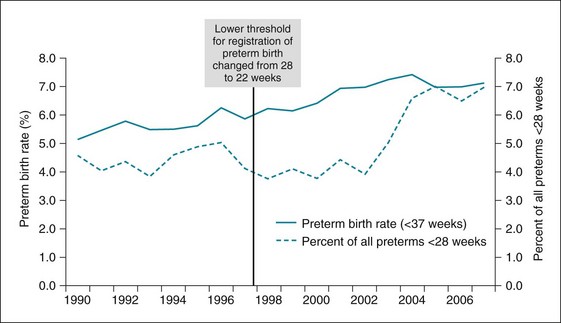
Figure 23-4 Variation in preterm birth rate and proportion of preterm births <28 weeks.
With a reduction in the lower threshold for registration of preterm births from 28 to 22 weeks of gestation in Denmark.
(From Blencowe H, Cousens S, Oestergaard M, et al: National, regional and worldwide estimates of preterm birth rates in the year 2010 with time trends for selected countries since 1990: a systematic analysis and implications. Lancet 379:2162–2172, 2012.)
In addition, some reports for birth outcomes exclude babies with congenital abnormalities, and others include only singleton births. These practices and perceptions vary between countries and over time, complicating the comparison of reported rates and interpretation of trends.24 Furthermore, methods for assessing gestational age vary between high-income and low-income countries and at least in high-income countries, have improved over time. Obstetric ultrasound is generally considered the standard of care in high-income countries,35 and although standardization remains a challenge, accuracy of gestational age assessment is better than in low-income countries.36,37 These variations in gestational age measurement methods further complicate the interpretation of preterm birth rates both within and between countries.
III Data Sources
A Vital Registration and Birth or Death Certificates
High coverage of vital registration through civil registration or certificates provides countries with data on numbers of births, deaths, and causes of death reasonably quickly. The time lag is usually 1 or 2 years.38 About 60% of the world’s births have a birth certificate, and while registration coverage has increased over the last decade, the countries with the most births and most deaths are least likely to have a high coverage of vital registration. However, vital registration coverage and quality have recently increased in some middle-income countries. About 81 countries now have vital registration systems with high coverage, accounting for only about 30% of the world’s births and about 26% of all deaths, and lower for neonatal mortality.39 Currently, birth certificates do not include “gestational age” and therefore cannot inform estimates of preterm birth rates.34
Death certificates are less often filled than birth certificates and less likely to be completed for stillbirths and early neonatal deaths compared to older children or adults. Until recently, many countries did not require stillbirth registration at all, and even in areas with high coverage, stillbirths are underreported.14,40–42 Furthermore, the quality of death certificate data varies significantly. Despite efforts to standardize death certificates both within countries and internationally, studies consistently demonstrate significant variability in reporting.
Clearly, the long-term solution is to improve registration systems to achieve high coverage of births and deaths. In the interim, demographic surveillance sites are another valuable source of data on trends, especially if selected to be nationally representative. Such sample registration systems are now used in China and India.43,44 In other countries, demographic surveillance sites that are not nationally representative may nevertheless provide useful data on mortality trends (http://www.indepth-network.org/). In the short-term, there is also a move to increase the frequency of UNICEF’s Multiple Indicator Cluster Surveys, using fewer questions and focusing on coverage of selected interventions, to provide more responsive data on program if not on mortality outcomes.45
B National Household Surveys and Censuses
Thus, to account for three quarters of the world’s births, we are dependent on other methods. The most important of these is the household survey, using a questionnaire to ask women about previous births and child deaths. This method has two major providers: DHS and MICS. Demographic and health surveys (DHS) are funded largely by U.S. government aid, but usually in partnership with national statistics offices,46 with data and results open access (www.measure.dhs.com). DHS report “under-five” mortality (children <5 years of age) and neonatal mortality rates for more than 80 countries, which account for two thirds of the world’s births.47 Some surveys also report data on stillbirth rates, but the quality of this reporting is variable. For the most recent Child Health Epidemiology Reference Group (CHERG/WHO) stillbirth rate, only about 50 countries had usable survey data, and 22 of 99 surveys were excluded based on quality criteria with implausible stillbirth rate/neonatal mortality rate (SBR/NMR) ratios. The United Nations International Children’s Emergency Fund (UNICEF) Multiple Indicator Cluster Surveys (MICS) address under-five mortality and coverage of interventions in many of the same countries, but these do not routinely analyze or report on stillbirths or neonatal deaths. Summary results are available (www.childinfo.org), but not the data sets.
Without household surveys, epidemiologists would have little idea of global child mortality or coverage of priority interventions, and their importance makes recognition of survey limitations essential. One important limitation is frequency. The expense and challenge of data collection and analysis in low-resource settings, using a survey tool with over 700 questions in the case of DHS, means that in most countries, surveys are only conducted every 5 years.48 Their ability to detect rapid changes in mortality or to disentangle contributory factors is therefore limited. This is important, especially in the context of the United Nations (UN) Millennium Development Goals (MDGs), which represent the widest commitment in history to addressing global poverty and ill (poor) health (http://www.un.org/millenniumgoals/).38,49 With increasing investment in maternal, newborn, and child health, governments and donors seek data capable of detecting short-term trends, particularly in the years up to 2015, the target for the MDGs.50 This would require huge increases in sample size. In Nigeria, for example, it would mean a fivefold expansion from the sample of 7225 households that already constitutes a major feat of organization.
Surveys, which depend on recall, also have particular limitations with respect to neonatal deaths and stillbirths, of which the most important is the potential for underascertainment of deaths compared with prospective surveillance. Systematic analyses of the extent of this problem are limited, but one study from rural India suggests that underreporting, especially in traditional societies, may halve the numbers of deaths reported.51 Even in transitional societies, early neonatal deaths are often unregistered, and stillbirths rarely so.52 Other issues of data quality include “age heaping” on certain days, notably days 7, 14, and 30, and miscoding between day 0 and day 1. Misclassification between stillbirths and early neonatal deaths, another important issue, was one of the arguments in favor of the combined measure of perinatal mortality, although expert opinion now favors separate reporting of stillbirths and neonatal deaths.4 More systematic analytic work is required to develop objective scores of data quality and transparent methods to correct for underreporting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree