Patient Story
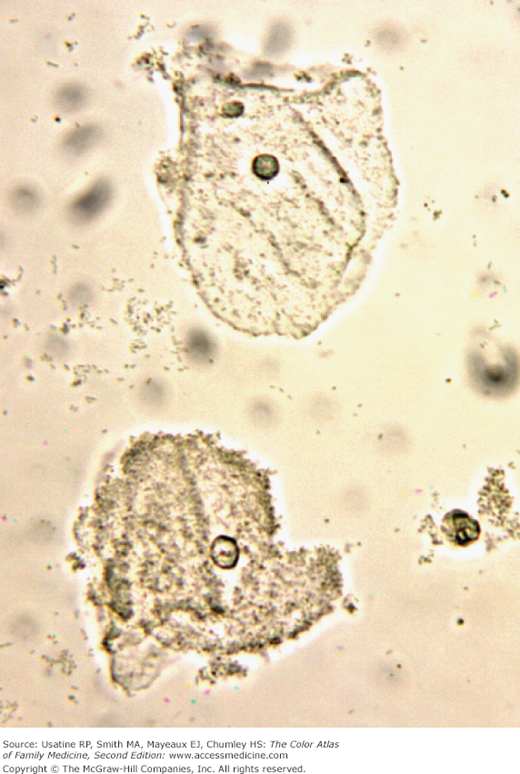
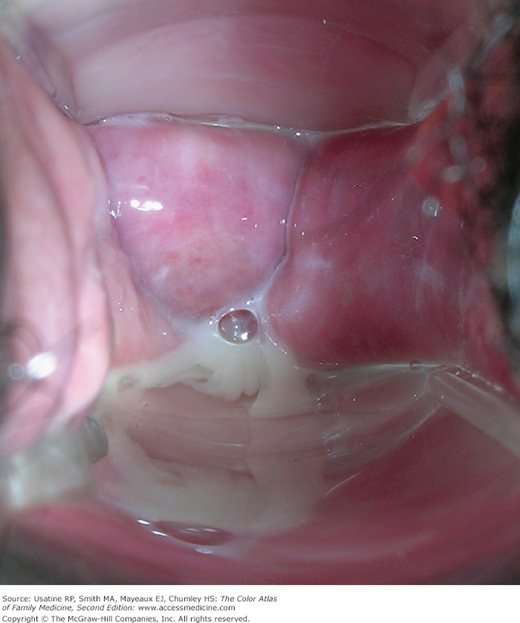
A 31-year-old woman presents with a malodorous vaginal discharge for 3 weeks. There is no associated vaginal itching or pain. She is married and monogamous. She admits to douching about once per month to prevent odor but it is not working this time. On examination, her discharge is visible (Figure 82-1). It is thin and off-white. Wet prep examination shows that more than 50% of the epithelial cells are clue cells (Figure 82-2). The patient is treated with oral metronidazole 500 mg bid for 7 days with good results.
Introduction
Bacterial vaginosis (BV) is a clinical syndrome resulting from alteration of the vaginal ecosystem. It is called a vaginosis, not a vaginitis, because the tissues themselves are not actually infected, but only have superficial involvement. Women with BV are at increased risk for the acquisition of HIV, Neisseria gonorrhoeae, Chlamydia trachomatis, and herpes simplex virus (HSV)-2, and they have increased risk of complications after gynecologic surgery.1
BV is associated with adverse pregnancy outcomes, including premature rupture of membranes, preterm labor, preterm birth, intraamniotic infection, and postpartum endometritis. However, the only established benefit of BV therapy in pregnant women is the reduction of symptoms and signs of vaginal infection.1
Synonyms
Epidemiology
Etiology and Pathophysiology
- Hydrogen peroxide-producing Lactobacillus is the most common organism composing normal vaginal flora.1 In BV, normal vaginal lactobacilli are replaced by high concentrations of anaerobic bacteria such as Mobiluncus, Prevotella, Gardnerella, Bacteroides, and Mycoplasma species.1,2
- The hydrogen peroxide produced by the Lactobacillus may help in inhibiting the growth of atypical flora.
- The odor of BV is caused by the aromatic amines produced by the altered bacterial flora in the vagina. These aromatic amines include putrescine and cadaverine—aptly named to describe their foul odor.
Risk Factors
Diagnosis
- Symptomatic patients present with an unpleasant, “fishy smelling” discharge that is more noticeable after coitus (the basic pH of seminal fluid is like doing the whiff test with KOH). There may be pruritus but not as often as seen with Candida vaginitis. The physical examination should include inspection of the external genitalia for irritation or discharge. Speculum examination is done to determine the amount and character of the discharge. A nucleic acid amplification test for N. gonorrhoeae, Chlamydia, and/or C. trachomatis (or similar test) should be performed on genital specimens (urethral or cervical) or urine.
- BV is usually clinically diagnosed by finding three of the following four signs and symptoms:
- Homogeneous, thin, white discharge that smoothly coats the vaginal walls (Figure 82-3 and 82-4).
- Presence of clue cells on microscopic examination (Figure 82-2).
- pH of vaginal fluid >4.5.
- A fishy odor of vaginal discharge before or after addition of 10% KOH (i.e., the whiff test).1
- Homogeneous, thin, white discharge that smoothly coats the vaginal walls (Figure 82-3 and 82-4).