B-cell Lymphoma, Unclassifiable, with Features Intermediate Between Diffuse Large B-cell Lymphoma and Classical Hodgkin Lymphoma
Francisco Vega, MD, PhD
Key Facts
Terminology
B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and CHL (DLBCL/CHL)
Clinical Issues
Most frequently presents as mediastinal mass
More aggressive clinical course than either CHL and PMLBCL
Microscopic Pathology
Overlapping histologic features that make classification difficult
Can exhibit confluent sheets of large cells resembling DLBCL
Can have scattered HRS-like cells resembling CHL
Ancillary Tests
Immunophenotype
Strong and uniform expression of B-cell antigens
CD30(+), CD45/LCA(+)
CD15 usually (−), EBV usually (−)
Top Differential Diagnoses
PMLBCL
Nodular sclerosis CHL
Diagnostic Checklist
In cases that morphologically resemble CHL
Uniform and strong expression of B-cell markers and absence of CD15 suggest DLBCL/CHL
In cases that morphologically resemble DLBCL
CD15(+), EBV(+), &/or CD20(−) suggest DLBCL/CHL
TERMINOLOGY
Abbreviations
B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma (DLBCL/CHL)
Synonyms
Gray zone lymphoma
Mediastinal gray zone lymphoma
Large B-cell lymphoma with Hodgkin features
Hodgkin-like anaplastic large cell lymphoma
Definitions
Lymphoma with clinical, morphologic, &/or immunophenotypic features between diffuse large B-cell lymphoma (DLBCL) and classical Hodgkin lymphoma (CHL)
CLINICAL ISSUES
Epidemiology
Age
Most common in patients 20-40 years or age (range: 13-70 years)
Gender
Male predominance
Ethnicity
Most common in Western countries
Less common in Asians and blacks
Presentation
Most frequently patients present with anterior mediastinal mass
Often direct extension into lungs
Supraclavicular lymph nodes can be involved
Advanced clinical stage (III or IV)
Other peripheral lymph node groups are rarely involved
Treatment
No consensus on optimum treatment protocol
Some patients treated with CHL protocols have failed to respond completely
Some groups have recommended treating DLBCL/CHL cases as aggressive DLBCL
Prognosis
Patients have aggressive clinical course and poorer outcome than patients with either CHL or primary mediastinal B-cell lymphoma
MICROSCOPIC PATHOLOGY
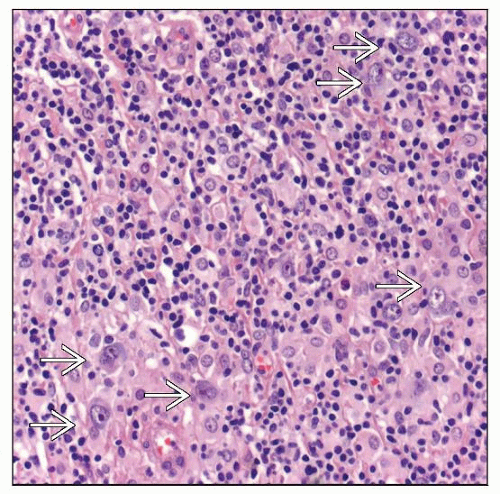
Histologic Features
Areas of confluent sheets of pleomorphic large tumor cells resembling DLBCL
Other areas can show scattered large cells, resembling Hodgkin and Reed-Sternberg (HRS) cells in CHL
Supraclavicular lymph nodes, if involved, can show morphologic features of either CHL or DLBCL or both
Variable inflammatory infiltrate in background
Mild stromal fibrosis and focal necrosis
Necrosis is usually not associated with neutrophils (unlike CHL)
Nonnecrotizing granulomas and histiocytes
Cytologic Features
Broad spectrum of cytologic appearance including
Centroblasts, immunoblasts, &/or HRS-like cells
Cells with cytoplasmic retraction, resembling lacunar cells, can be seen
Mummified cells (apoptotic large cells) are frequent
ANCILLARY TESTS
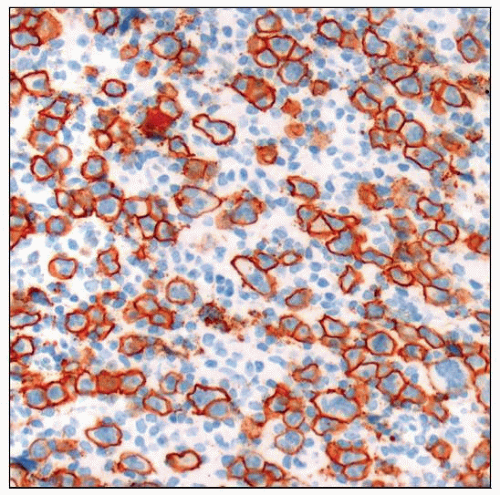
Immunohistochemistry
“Mixed immunophenotype” with
Expression of common markers of classical HL
CD30([+] all cases) &/or CD15([+] in most cases)
pax-5(+) and IRF-4/MUM-1(+)
And expression of markers usually absent in CHL
CD45/LCA(+), CD20 ([+]; uniformly strong), and CD79a(+)
OCT2(+), BOB1(+)
Cells with this “mixed immunophenotype” constitute predominant neoplastic cell population
Usually high proliferation rate, as measured by MIB-1 (Ki-67)
MAL(+) in ˜ 60% of cases
Bcl-6([+] variable), CD10 is usually (−)
Negative for T-cell markers, ALK(−)
Epstein-Barr virus (EBV) is usually (−)
Few cases reported were EBV(+); EBER &/or LMP1
Like CHL, lymphoid infiltrate in background is predominantly composed of T cells, CD3(+) and CD4(+)
These cases show immunohistochemical features supporting activation of NF-κB pathway
Nuclear location of c-REL/p65
Overexpression of phosphorylated IκBa
Overexpression of NF-κB targets, Bcl-XL, and c-FLIP
Molecular Genetics
Most cases have monoclonal IgH gene rearrangement
Few cases have rearrangements involving BCL6
Most cases lack t(14;18)(q32;q21)
In almost all cases assessed, P53 was in germline configuration
Gene Expression Profiling
Studies have shown similarity between CHL and primary mediastinal large B-cell lymphoma
This is theoretical support for category of DLBCL/CHL
However, few cases of DLBCL/CHL have been analyzed by gene expression profiling
DIFFERENTIAL DIAGNOSIS
Primary Mediastinal (Thymic) Large B-cell Lymphoma (PMLBCL)
Usually young women
Anterosuperior mediastinal mass (rapidly progressive)
Patients can have extrathoracic disease
Rare at time of diagnosis
More common at time of relapse
Usually extranodal: CNS, liver, adrenals, ovaries, and kidneys
Lymph nodes are often not involved at relapse
Histologic features
Diffuse growth pattern
Large cells with pale cytoplasm (often is retraction artifact)
Sclerosis
Often compartmentalizes tumor cells mimicking cohesive clusters
Reed-Sternberg-like or Hodgkin-like cells can be present
Immunophenotype
Positive for common pan B-cell markers
CD20(+), CD79a(+), pax-5(+)
CD45/LCA(+), IRF-4/MUM-1(+)
CD30([+] 80%), usually weak &/or focal
CD23([+] 70%), MAL([+] 70%)
Often surface immunoglobulin(−); best shown by flow cytometry
CD10(−), CD15(−)
EBV is usually (−)
T-cell antigens(−)
Molecular genetic features
Monoclonal Ig gene rearrangements are present
No evidence of monoclonal TCR gene rearrangements
Array CGH shows amplification at 9p24 (˜ 75%) and 2p15 (˜ 50%)
These neoplasms show a number of deletions
Nodular Sclerosis Classical Hodgkin Lymphoma
Usually young patients
Slight female predominance
Mediastinal involvement (˜ 80%)
Histologic features
Nodular growth pattern with fibrosis
Dense collagenous bands surround nodules
Collagenous bands are polarizable
Variable number of large HRS cells
Many histological variants of nodular sclerosis CHL have been described
Based on number of neoplastic cells, extent and nature of fibrosis, and inflammatory background
Of these, syncytial variant is particularly relevant in differential diagnosis
Sheets of large tumor cells that can mimic DLBCL
Often large areas of necrosis
Immunophenotype is typical of CHL
Immunophenotype
CD30(+), CD15(+) in most cases
pax-5(+) with characteristic weaker (dimmer) expression than reactive B-cells
CD20(−/+), CD79a(−/+)
Weakly &/or variably (+) in ˜ 20% of cases
Small subset (˜ 5%) of CHL can express T-cell antigens
These cases also express pax-5 or other B-cell antigens
CD45/LCA(−), EMA usually (−)
Molecular genetic features
Monoclonal IgH gene rearrangements usually only detected by single cell PCR
Usually no evidence of monoclonal Ig or TCR gene rearrangements by routine analysis
Standard PCR performed on whole tissue sections
Southern blot analysis
Diffuse Large B-cell Lymphoma
Older adults, but also occurs in children and young adults
Histologic features
Diffuse growth pattern
Large neoplastic cells (centroblasts &/or immunoblasts)
Large anaplastic cells can be present; known as anaplastic variant
These neoplasms may have intrasinusoidal growth pattern
CD30 often (+)
Large pleomorphic cells with features of HRS-like cells can be present
Sclerosis is frequent in extranodal sites
Areas of coagulative necrosis are common
Immunophenotype
CD20(+), CD22(+), CD79a(+)
pax-5(+), OCT2(+), BOB1(+)
CD10(+) and Bcl-6(+) in variable proportion of cases
CD30(−/+); if positive, often weak and focal except anaplastic variant
CD45/LCA(+), CD15(−)
Monotypic immunoglobulin(+)
Cytoplasmic; in cases with plasmacytoid differentiation
Surface; best shown by flow cytometry
Molecular genetic features
Monoclonal Ig gene rearrangements(+)
No evidence of monoclonal TCR gene rearrangements
t(14;18)(q32;q21)/IgH-BCL2 (+) in ˜ 20-30%
BCL6 rearrangements in ˜ 10-20%
Gene expression profiling has shown 2 subsets
Germinal center cell
Activated B cell
Poorer prognosis
ALK(+) Anaplastic Large Cell Lymphoma (ALCL)
Children and young adults
Male predominance
Mediastinal involvement is rare
Histologic features
Diffuse &/or sinusoidal growth pattern
Large, irregular neoplastic cells and “hallmark cells”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree