B-cell Lymphoma, Unclassifiable, with Features Intermediate Between Diffuse Large B-cell Lymphoma and Burkitt Lymphoma
Carlos E. Bueso-Ramos, MD, PhD
Key Facts
Terminology
Aggressive B-cell lymphoma with morphological and genetic features of both DLBCL and BL
WHO classification considers this category
Heterogeneous and not distinct entity
Clinical Issues
Median age: 6th decade
Patients present with lymphadenopathy &/or extranodal masses; high stage in > 50%
Aggressive clinical course for most patients
Current chemotherapy regimens are ineffective
Microscopic Pathology
Diffuse growth pattern; “starry sky” pattern is common
High mitotic and apoptotic rates
Intermediate-sized cells or a spectrum of cell sizes
Ancillary Tests
Pan-B-cell antigens(+): TCL1(+/−), Ki-67 high
In cases with immunophenotype consistent with BL
CD10(+), Bcl-6(+), IRF-4/MUM1(−), Bcl-2(−)
In double-/triple-hit lymphomas, Bcl-2 is strongly (+)
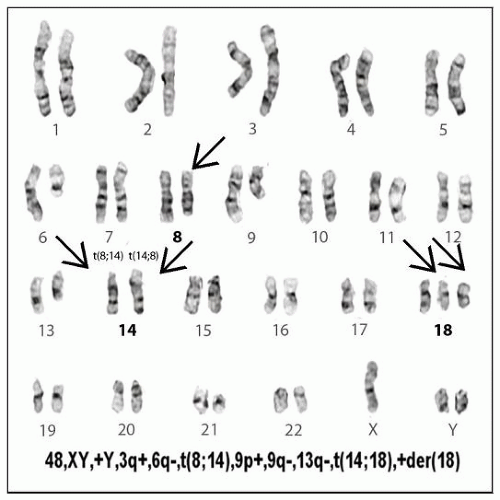
Complex karyotype is common
MYC translocations in up to 50% of all cases
Associated with BCL2 &/or BCL6 rearrangements in double-/triple-hit lymphomas
Top Differential Diagnoses
Burkitt lymphoma
Diffuse large B-cell lymphoma
Lymphoblastic leukemia/lymphoma
Mantle cell lymphoma, blastoid variant
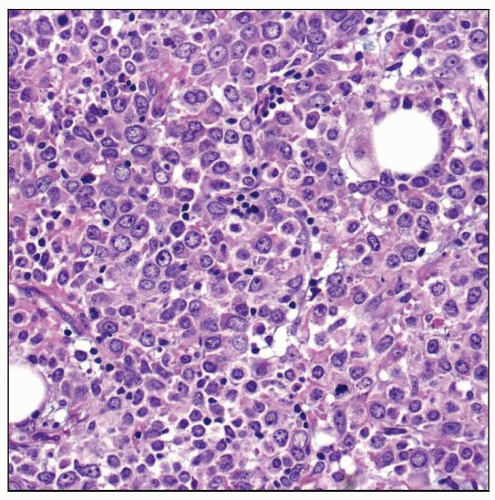 B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and BL (DLBCL/BL). Note the high number of apoptotic cells and the mixture of intermediate and large-sized cells. |
TERMINOLOGY
Abbreviations
B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL)
Synonyms
Burkitt-like lymphoma
High-grade B-cell lymphoma, Burkitt-like (Revised European American Lymphoma [REAL] classification)
Small noncleaved cell lymphoma, non-Burkitt (Working Formulation)
Definitions
Aggressive B-cell lymphoma with morphological and genetic features of both DLBCL and BL
World Health Organization (WHO) classification considers this category
Heterogeneous and not distinct entity
Useful as “parking lot” for unclassifiable high-grade B-cell lymphomas
ETIOLOGY/PATHOGENESIS
Unknown
Subset of DLBCL/BL cases includes “double-hit” or “triple-hit” lymphomas
“Hit” in this context refers to translocations involving MYC, BCL2, or BCL6 genes
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon, but true frequency not yet known
Frequency increases with patient age
Age
Adults; median: 6th decade
Gender
Males > females
Site
> 50% of patients present with disseminated disease
Lymph nodes
Extranodal sites common and include
Bone marrow (˜ 50%) and brain (˜ 33%)
Presentation
Patients present with lymphadenopathy &/or extranodal masses
˜ 10-20% of patients have history of follicular lymphoma
B-type symptoms common
Leukemic presentation uncommon but can occur
Laboratory Tests
Elevated serum lactate dehydrogenase &/or β-2-microglobulin levels
Elevated leukocyte count with lymphoma cells in patients with leukemic presentation
Natural History
Aggressive clinical course for most patients
Poor prognostic factors
High clinical stage
Central nervous system involvement
History of follicular lymphoma
Double- or triple-hit lymphoma
Treatment
Drugs
No consensus on optimal therapeutic approach
Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) usually not effective
Rituximab, hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-HyperCVAD) effective for subset of patients
Prognosis
DLBCL/BL is heterogeneous and therefore prognosis is also heterogeneous
Large subset of patients have poor clinical outcome despite rigorous chemotherapy regimen
IMAGE FINDINGS
CT Findings
F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT)
DLBCL/BL is highly FDG avid
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse growth pattern; “starry sky” is common
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree