Atypical (Dysplastic) Melanocytic Nevi
Soheil Sam Dadras, MD, PhD
Olubukola Babalola
Key Facts
Terminology
Pigmented lesion with clinical, architectural, and cytologic atypia, characterized into familial and sporadic dysplastic nevi
Dysplastic nevus, B-K mole, Clark nevus
Clinical Issues
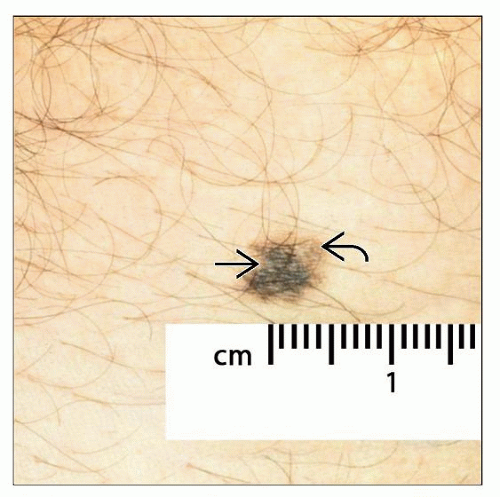
Typically > 6 mm in diameter (range: 8-10 mm)
Variegate pigmentation with irregular borders
Central papule with peripheral macular flare or fuzzy appearance
Microscopic Pathology
Presence of shouldering phenomenon
Lamellar and concentric fibroplasia
Range of cytologic atypia
Enlarged cells with dusky, abundant cytoplasm
Nuclear pleomorphism (mild to severe)
Small to prominent nucleoli
Top Differential Diagnoses
Common acquired nevus
May show some shouldering, but no melanocytes proliferating to peripherally expand rete
Congenital melanocytic nevus
Often have a greater intradermal than junctional component
Band-like distribution of intradermal cells surrounded by adnexal structures
Malignant melanoma
Lack of symmetry and circumscription
Lack of maturation with increasing dermal depth
Often show mitoses and marked nuclear atypia, with irregular chromatin and large nucleoli
TERMINOLOGY
Abbreviations
Atypical melanocytic nevus (AMN)
Synonyms
Dysplastic nevus, B-K mole, Clark nevus
Definitions
Pigmented lesion with clinical, architectural, and cytologic atypia, which may be separated into familial and sporadic atypical/dysplastic nevi
Controversial entity, as some believe that it may represent only another type of nevus, given the overlapping clinicopathological features that exist between it and common acquired melanocytic nevi
CLINICAL ISSUES
Epidemiology
Age
Adolescents to young and old adults
Site
Any location may be involved (especially those with familial type)
Including scalp, doubly covered areas (breasts in women and bathing trunk area in men and women), and lower legs
Presentation
Papule, typically 8-10 mm
Irregular borders
Variegate pigmentation
Central papule with peripheral macular flare or fuzzy border
Treatment
Surgical approaches
Simple excision for moderately atypical melanocytic nevi
Excision with 5 mm clinical margins for severely atypical nevi
Prognosis
Once adequately excised, should have very low risk of local recurrence; little, if any, risk of melanoma
MICROSCOPIC PATHOLOGY
Histologic Features
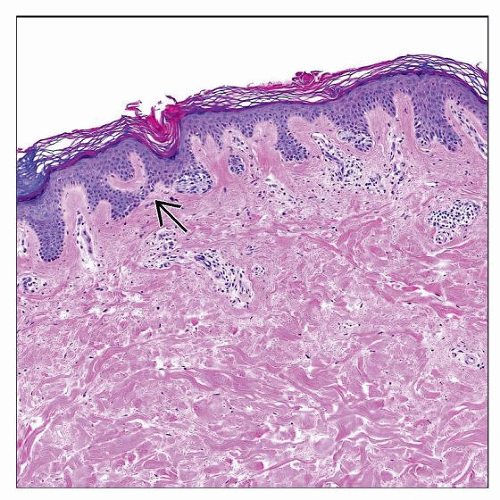
Junctional or compound nevus with architectural disorder and asymmetry
Presence (extension) of peripheral nests beyond dermal component (shoulder phenomenon) in compound nevi, typically 3 rete ridges beyond center of lesion
Lentiginous proliferation of melanocytes that fuse (bridge across) adjacent rete ridges via proliferation of single cells and nests
Pagetoid scatter may be focally present, but usually limited to center of lesion
Subepidermal lamellar (stacked) fibroplasia parallel to epidermis
Circumferential fibroplasia surrounding nests
Vascular proliferation in reticular dermis
Chronic inflammation with melanophages in dermis
Cytologic Features
Ample brown-gray cytoplasm
Nuclear pleomorphism (greater in more moderate- and severe-grade lesions)
Nuclear diameter larger than mid-layer epidermal keratinocyte, especially in moderately to severely atypical lesions
Densely hyperchromatic chromatin pattern
Nucleolar prominence (greater in higher grade lesions)
DIFFERENTIAL DIAGNOSIS
Common Acquired Nevus
May exhibit some shouldering of junctional component
No melanocytes proliferating to peripherally expand rete
Lacks significant cytological atypia and mitotic activity
Congenital Melanocytic Nevus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree