Patient Story
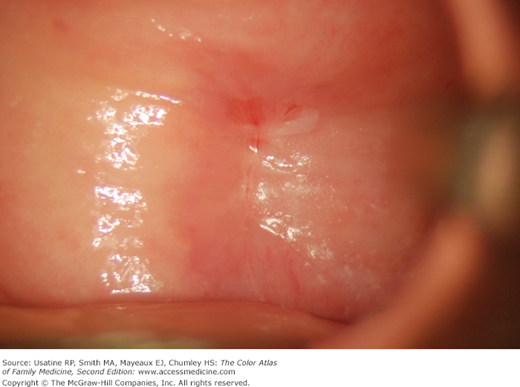
A 60-year-old woman with vaginal dryness and irritation is seen to follow-up on an inflammatory Pap smear. She denies discharge, odor, douching, and sexually transmitted disease (STD) exposure. She does admit to some postcoital bleeding. Her cervix has atrophic changes and an endocervical polyp (Figure 81-1). The polyp was removed easily with a ring forceps and no dysplasia was found on pathology.
Introduction
Epidemiology
- The average age of menopause is 51 years in the United States.
- Approximately 5% of women experience menopause after age 55 years (late menopause), and another 5% experience the transition between the ages of 40 and 45 years (early menopause). This means that in the United States, most women will live a significant portion of their lives during menopause. Women who in menopause have surgical menopause or have ovarian suppression without estrogen supplementation (progestin-only contraceptives) are susceptible to atrophic changes in their lower genital tract.
- Vaginal dryness occurs in approximately 3% of women of reproductive age, 4% to 21% of women in the menopausal transition, and 47% of women 3 years postmenopause.1 Internationally, 39% of women experience menopause-related vaginal discomfort.2
Etiology and Pathophysiology
- After menopause, circulating estrogen levels dramatically decrease to a level at least one-sixth their premenopausal levels.3 Changes that occur in the vaginal and cervical epithelium include proliferation of connective tissue, loss of elastin, thinning of the epithelium (Figure 81-2), and hyalinization of collagen.
- A long-term decrease in estrogen is generally necessary before symptoms become apparent. Genital symptoms include decreased vaginal lubrication, dryness, burning, dyspareunia, leukorrhea, itching, and yellow malodorous discharge.
- Urinary symptoms, such as frequency, hematuria, urinary tract infection, dysuria, and stress incontinence, are usually late symptoms. Over time, the lack of vaginal lubrication often results in sexual dysfunction.
- Cervical polyps (Figure 81-1) are pedunculated tumors that usually arise from the endocervical canal mucosa, and are common in patients with atrophic vaginitis. Many will show squamous metaplasia, and they may develop squamous dysplasia. Polyps are most commonly asymptomatic unless they bleed.
- Menopause is the most common cause of atrophic vaginitis. In premenopausal women, radiation therapy, chemotherapy, immunologic disorders, and oophorectomy may greatly decrease production of ovarian estrogen and lead to atrophic vaginitis. Antiestrogen medications may also result in atrophic vaginitis. Women who are naturally premenopausally estrogen deficient, smoke cigarettes, or have not given vaginal birth tend to have more severe symptoms.3
Risk Factors
- Age.
- Family history of early menopause.
- Bilateral oophorectomy.
- Spontaneous premature ovarian failure.
- Antiestrogenic medications effects, such as tamoxifen, danazol, medroxyprogesterone acetate.
- Gonadotropin-releasing hormone agonists (leuprolide, nafarelin, goserelin), or antagonists (ganirelix).
- Prolactin elevation as a result of hypothalamic-pituitary disorders with secondary reduction of estrogen secretion.
- Certain chemotherapeutic agents.
- Pelvic radiation therapy.
- Severe systemic lupus erythematosus or rheumatoid arthritis (because of hypothalamic hypogonadism or primary ovarian insufficiency) combined with glucocorticoid therapy cause combined suppression of ovarian and adrenal activity.
Diagnosis
- Diagnosis is clinical, based upon characteristic symptoms and findings. Many women with symptoms of vaginal atrophy do not discuss their condition with a health care provider because they believe their symptoms are a normal part of the aging process.4
- Atrophic vaginal and cervical epithelium appears pale, smooth, relatively dry, and shiny (Figure 81-2). Inflammation with patchy erythema, petechiae, and friability is common in more advanced cases. The external genitalia may demonstrate diminished elasticity, turgor of skin, sparsity of pubic hair, dryness of labia, erythema (Figure 81-3), and fusion of the labia minora.5