• Chronic, pruritic, inflammatory skin condition • Skin is dry and hyperkeratotic • Lesions include excoriations, papules, eczema (patches of erythema, exudation, and scaling with small vesicles formed within the epidermis), and lichenification (hyperpigmented plaques of thickened skin with accentuated furrows) • Scratching and rubbing lead to lichenification, most commonly in the antecubital and popliteal flexures Common condition (2.4%-7% of population). • Immediate hypersensitivity disease: serum immunoglobulin E is elevated in 80% of patients. All patients have positive skin, radioallergosorbent test, and other allergy tests. Positive family history in two thirds of patients. Many develop allergic rhinitis and/or asthma. Most improve with elimination diet. • Physiologic and anatomic abnormalities of skin: type of abnormality determines manner in which atopic dermatitis (AD) is manifested in each patient: lowered threshold to itch stimuli (substance P excess?); hypersensitivity to alpha-adrenergic agonists and cholinergic agents by partial beta-adrenergic blockade (receptor site insensitivity); dry, hyperkeratotic skin with decreased water-holding capacity (dry: zinc or thyroid deficiency; hyperkeratotic: vitamin A deficiency?); tendency to lichenify in response to rubbing and scratching (membrane fragility?); skin heavily colonized by bacteria (coagulase-positive Staphylococcus aureus) (immune dysfunction). • Dennie’s sign: accentuated double pleat below margin of lower eyelid and tendency toward vasoconstriction provoked by physical pressure (“white dermatographism”). • Predictors of severity in children: eczema starting during the first year of life, a history of atopy (asthma, hay fever, or both), and urban living (independent of ethnicity) increase risk of severe disease. • Immunologic abnormalities: leukocytes have decreased cyclic adenosine monophosphate (cAMP) from increased cAMP-phosphodiesterase activity and decreased prostaglandin precursors. Decreased intracellular cAMP increases histamine release and decreases bactericidal activity. • Defect in serum bactericidal activity (alternate complement pathway [ACP]): inulin-containing herbs (burdock root [Arctium lappa] and dandelion root [Taraxacum officinale]) may restore bactericidal activity and increase cAMP. Inulin activates ACP. • Predominance of pathogenic Staphylococcus aureus in skin flora in 90% of patients, increasing susceptibility to Staphylococcus infections. • Cell-mediated immunity defects: increase susceptibility to cutaneous herpes simplex, vaccinia, molluscum contagiosum, and verruca vulgaris infections. Others include reduced delayed-type hypersensitivity, cutaneous anergy, and decreased in vitro lymphocyte reactivity to mitogens and antigens. Cell-mediated defects normalize during remission and become abnormal again during recurrences. • Food allergy: plays a major role in AD (Textbook, “Atopic Dermatitis [Eczema]”). Breastfeeding acts as prophylaxis against AD (and allergies in general). Breastfed infants develop AD as a result of transfer of antigens in breast milk. Mothers should avoid common food allergens (milk, eggs, peanuts, fish, soy, wheat, citrus, and chocolate). In older or formula-fed infants, milk, eggs, and peanuts are the most common foods inducing AD. Virtually any food can be offending agent. Food allergy is best diagnosed by elimination diet and challenge. Lab methods to identify food allergens in eczema: enzyme-linked immunosorbent assay for immunoglobulin (Ig) E and IgG4 (Textbook, “Food Reactions”). Food allergies are linked to “leaky gut,” that is, increased gut permeability with increased antigen load on immune system and developing additional allergies. Eliminating allergenic foods can stop development of new allergies. Avoiding offending foods for 1 year may eradicate allergy; loss rate after 1 year is 26% for five major allergens (egg, milk, wheat, soy, peanut) and 66% for other foods. • Candida albicans: gastrointestinal overgrowth is a causative factor in allergies, including AD. Elevated anti-Candida antibodies are common in atopy. Severity of lesions correlates with level of IgE antibodies to Candida; anti-Candida therapy (Textbook, “Atopic Dermatitis [Eczema]”) may significantly improve AD. Intestinal flora play major role in AD; probiotics are especially indicated. Lactobacillus rhamnosus GG, alone or with Lactobacillus reuteri, reduces severity in infants with AD and cow’s milk allergy. Positive effect of probiotics is more pronounced in patients with allergic constitution (positive skin prick test). • Essential fatty acids and prostaglandin metabolism: AD patients have altered essential fatty acid (EFA) and prostaglandin metabolism: increased linoleic acid levels with decreased longer-chain polyunsaturated fatty acids (gamma-linolenic acid and arachidonic acid) and omega-3s (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]). Proportions of linoleic acid in total plasma lipids and phospholipids are greater, and those of oleic acid lower, than normal in AD patients. Ratio of omega-3 to omega-6 fatty acids is lower in AD patients. Lack of significant decreases in proportions of dihomo-gamma-linolenic acid and arachidonic acid observed in plasma lipids of AD patients suggests that delta-6-desaturase is not impaired. Fish oil, providing EPA and DHA, or simply eating more wild fatty fish (mackerel, herring, salmon) increases omega-3 fatty acids in membrane phospholipids. Degree of clinical improvement correlates with increased DHA in serum phospholipids; fish oils are more effective in raising DHA than is flaxseed oil; EPA/DHA supplements or increasing consumption of wild cold-water fish may produce better results than flaxseed oil. • Inhibiting excess histamine release: agents that stimulate cAMP production and/or inhibit cAMP phosphodiesterase reduce inflammatory process in AD by reducing shunting to histamine. Coleus forskohlii strongly enhances cAMP. Many botanicals inhibit diesterase; licorice (Glycyrrhiza glabra) shows marked activity. Flavonoids also inhibit cAMP phosphodiesterase: quercetin and hyperoside, the flavones orientin and vitexin, and the flavanone naringen. The common flavanol, rutin, has <1/10 activity of quercetin. Flavonoid extracts from Vaccinium myrtillus, Rosa damascena, Ruta graveolens, Prunus spinosa, and Crataegus pentagyna are the most potent inhibitors of cAMP phosphodiesterase and also inhibit mast cell degranulation. Flavonoid-rich extracts (grape seed, pine bark, green tea, Ginkgo biloba) may prove helpful. Ginkgo terpenes (ginkgolides) antagonize platelet-activating factor (PAF), a key mediator in AD. PAF plays central role in neutrophil activation, increasing vascular permeability and smooth muscle contraction (bronchoconstriction), and reducing coronary blood flow. Ginkgolides compete with PAF for binding sites. Mixtures of ginkgolides and Ginkgo biloba extract (standardized to 24% ginkgo flavonglycosides and 6% terpenoids) demonstrate significant antiallergy effects. • Zinc: low Zn is common in AD. EFA metabolism is essential in AD (Zn required for delta-6-desaturase). • Vitamin E: 400 IU q.d. for 8 months significantly improved 60% of patients, with significant reductions in serum IgE.
Atopic Dermatitis (Eczema)
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
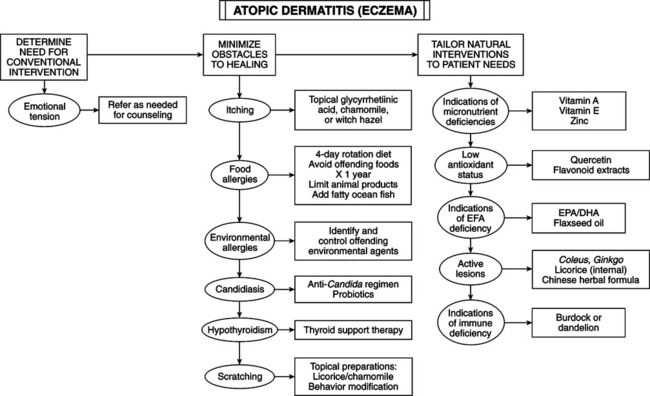
THERAPEUTIC CONSIDERATIONS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
