Patient Story
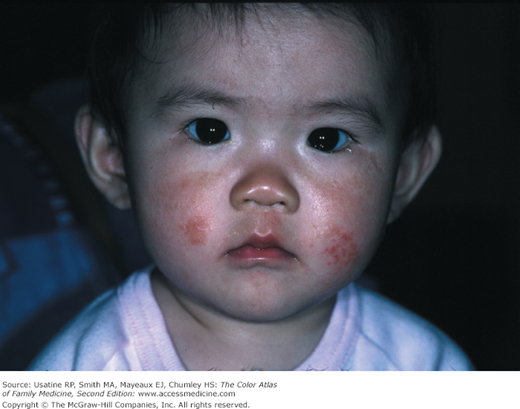
A 1-year-old Asian American girl is brought to her family physician for a new rash on her face and legs (Figures 145-1 and 145-2). The child is scratching both areas but is otherwise healthy. There is a family history of asthma, allergic rhinitis, and atopic dermatitis (AD) on the father’s side. The child responded well to low-dose topical corticosteroids and emollients.
Figure 145-2
Atopic dermatitis on the leg of the infant in Figure 145-1. The coin-like pattern is that of nummular eczema. (With permission from Milgrom EC, Usatine RP, Tan RA, Spector SL. Practical Allergy. Philadelphia, PA: Elsevier; 2004.)
Introduction
Epidemiology
- AD is the most frequent inflammatory skin disorder in the United States and the most common skin condition in children.1
- Worldwide prevalence in children is 15% to 20% and is increasing in industrialized nations.2
- Sixty percent of cases begin during the first year of life and 90% by 5 years of age.1 One third will persist into adulthood.2
- Sixty percent of adults with AD have children with AD (Figure 145-3).1
Etiology and Pathophysiology
- Strong familial tendency, especially if atopy is inherited from the maternal side.
- Associated with elevated T-helper (Th) 2 cytokine response, elevated serum immunoglobulin (Ig) E, hyperstimulatory Langerhans cells, defective cell-mediated immunity, and loss of function mutation in filaggrin, an epidermal barrier protein.
- Exotoxins of Staphylococcus aureus act as superantigens and stimulate activation of T-cells and macrophages, worsening AD without actually showing signs of superinfection.
- Patients may have a primary T-cell defect. This may be why they can get more severe skin infections caused by herpes simplex virus (eczema herpeticum as seen in Figure 145-4) or bacteria (widespread impetigo). They are also at risk of a bad reaction to the smallpox vaccine with dissemination of the attenuated virus beyond the vaccination site. Eczema vaccinatum is a potentially deadly complication of smallpox vaccination (Figure 145-5).
Diagnosis
- History—Pruritus is the hallmark symptom of AD. It is referred to as “the itch that rashes” as patients will often feel the need to scratch before a primary lesion appears. If it does not itch, it is not AD. Persons with AD often have a personal or family history of other allergic conditions, namely asthma and allergic rhinitis.
- The atopic triad is AD, allergic rhinitis, and asthma. Atopic persons have an exaggerated inflammatory response to factors that irritate the skin.
- Physical examination—Primary lesions include vesicles, scale, papules, and plaques.
- Secondary (or sequential) lesions include linear excoriations from scratching or rubbing which may result in lichenification (thickened skin with accentuation of skin lines), fissuring, and prurigo nodularis. Crust may indicate that a secondary infection has occurred. Postinflammatory hyperpigmentation and follicular hyperaccentuation (more prominent hyperkeratotic follicles) (Figure 145-6) may also be identified.
- AD often starts on the face in infancy and childhood (Figures 145-1 and 145-7) and then appears in the flexural folds, especially the antecubital and popliteal fossa (Figures 145-8, 145-9, 145-10).
- Involvement of the neck, wrists, and ankles also may occur (Figures 145-11 and 145-12).
- AD in adults can occur on the hands, around the mouth, or eyelids as well as all the other areas (Figures 145-13 and 145-14).
- In one series, the prevalence of hand involvement in patients with active AD was 58.9%. There was a significant trend toward an increasing prevalence of hand involvement with increasing age.3