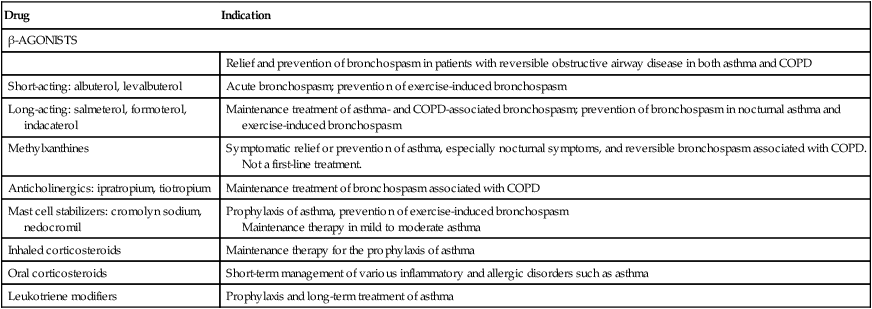
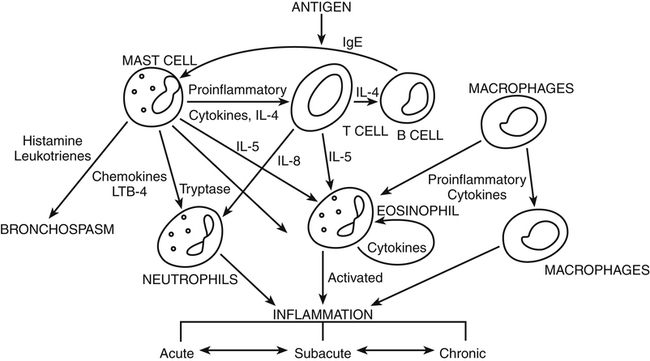
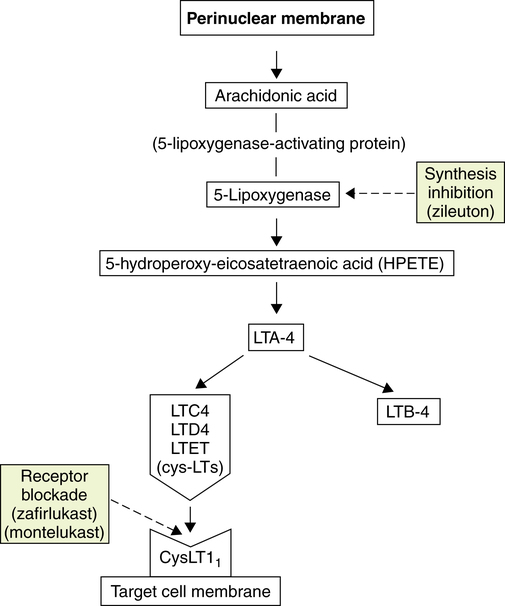
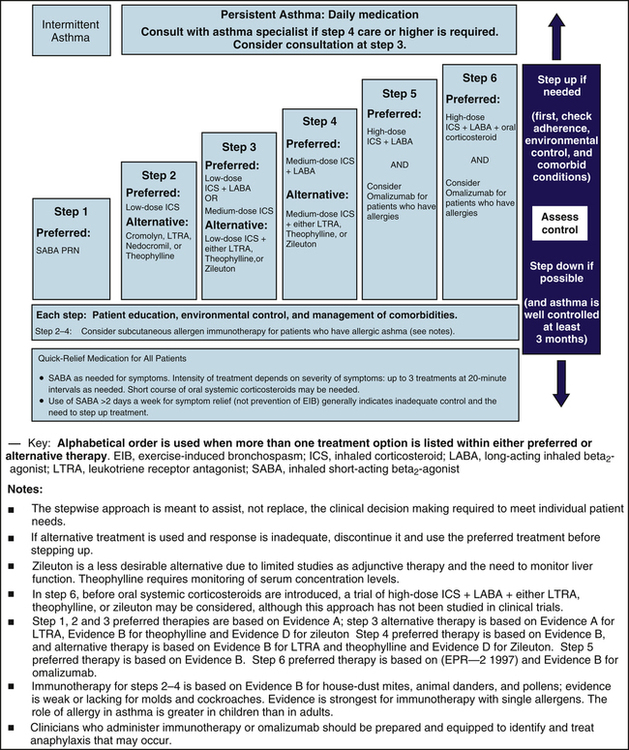
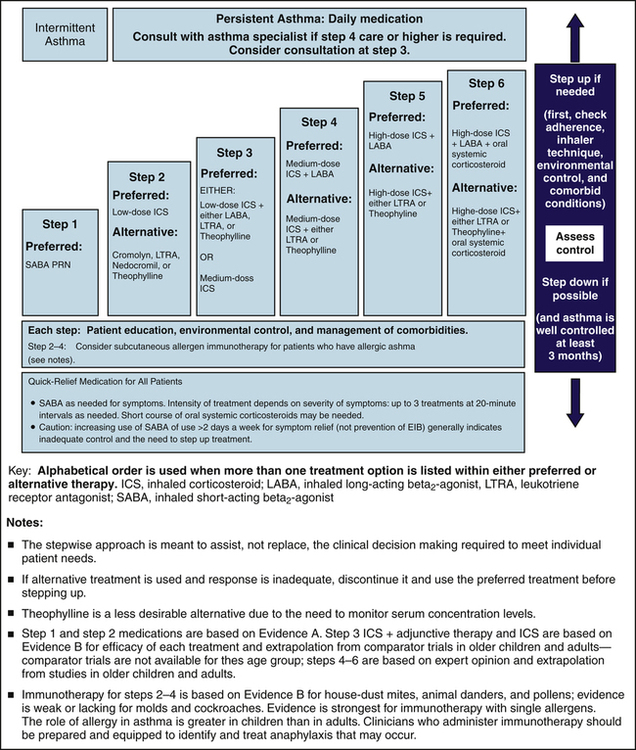
Chapter 16 The lungs also contain α-adrenergic receptors, and their stimulation results in mild bronchoconstriction. No β1-adrenergic receptors are present in the lungs. β1-adrenergic receptors are the predominant adrenergic receptors of the heart, and their stimulation promotes myocardial contractility and conduction, resulting in an increased heart rate (Table 16-2). TABLE 16-2 Location and Response of Adrenoreceptors Modified from Lees GM: A hitchhiker’s guide to the galaxy of adrenoreceptors, BMJ 283:173-178, 1981. • Airway hyperresponsiveness: The airways react abnormally to some triggers such as inhaled allergens, food or recreational drugs, aspirin and related NSAIDs, cold air, exercise, airway irritants (e.g., cigarette smoke, air pollution), respiratory infection, and emotional stress. Conditions such as GERD, chronic sinusitis, and rhinitis also can exacerbate asthma. • Airway inflammation: On exposure to an inhaled antigen, mast cells, eosinophils, epithelial cells, macrophages, and activated T-cells are released. The chemical mediators that they release consist of cytokines, chemokines, histamine, prostaglandins, and leukotrienes (LTs). Their response in the airways occurs as bronchospasm and inflammation (Figure 16-1); see Chapter 68 on the immune system for additional details. • Airway obstruction: Bronchoconstriction results in a decline in the forced expiratory volume in 1 second (FEV1). Inflammatory processes occur within the bronchiole, causing epithelial injury. Chronic inflammation can lead to airway remodeling, thickening of goblet cells, mucous hypersecretion, thickening of the basement membrane by collagen deposition, and hypertrophy of smooth muscle, all of which contribute to airway obstruction. In the case of longstanding asthma, symptoms may not be reversible due to airway remodeling. 1. Intermittent: Symptoms ≤2 days per week, symptoms that cause nighttime awakenings ≤2 nights per month, no interference with normal activity, FEV1 >80% of predicted, and FEV1/FVC normal. 2. Mild persistent: Symptoms >2 days per week but not daily, symptoms that cause nighttime awakenings 3 to 4 times a month, minor limitation of function, FEV1 >80% of predicted, and FEV1/FVC normal. 3. Moderate persistent: Daily daytime symptoms, symptoms that cause nighttime awakenings >1 time per week but not nightly, some limitation in function, FEV1 >60% but <80% of predicted, and FEV1/FVC reduced by 5%. 4. Severe persistent: Continuous daytime symptoms, symptoms that occur nightly, extremely limited activity, FEV1 <60% of predicted, and FEV1/FVC reduced by >5%. • Stage I (mild COPD): FEV1/FVC <0.70, FEV1 ≥80% of predicted • Stage II (moderate COPD): FEV1/FVC < 0.70, FEV1 50% to 79% of predicted • Stage III (severe COPD): FEV1/FVC <0.70, FEV1 30% to 49% of predicted • Stage IV (very severe COPD): FEV1/FVC ≤0.70, FEV1 ≤30% of predicted or <50% of predicted plus chronic respiratory failure Corticosteroids modify the body’s immune responses to various stimuli. They suppress cytokine production, airway eosinophil recruitment, and the release of inflammatory mediators. Inhaled corticosteroids (ICSs) provide local therapeutic action with minimal systemic effects. (See Chapter 51 for a detailed discussion of mechanism of action.) ICSs have been shown to reduce asthma symptoms, improve quality of life, improve lung function, decrease airway hyperresponsiveness, control airway inflammation, reduce frequency and severity of exacerbations, and reduce asthma mortality. Oral corticosteroid treatment often is indicated for exacerbation of asthma and some cases of COPD. ICS therapy in COPD does not alter the course of the disease but does control symptoms and has been shown to reduce the frequency of exacerbations. Cysteinyl LTs (cysLTs) are more potent and longer-acting bronchoconstrictors than histamine. They are produced in a variety of cells (e.g., eosinophils, mast cells, basophils, macrophages, and monocytes) from arachidonic acid through several enzyme pathways (Figure 16-2). Arachidonic acid is released from cell membranes in response to antigen–antibody reactions, immunoglobulin (Ig)E receptor activation, microorganisms, and physical stimuli. LTs enhance responsiveness of the airways to a variety of stimuli and stimulate secretion of mucus in the airways. Zafirlukast and montelukast are potent competitive leukotriene receptor antagonists (LTRAs). They block the action of cysLTs at receptor sites on smooth muscle cells throughout the bronchioles. A single type of receptor is able to mediate profound contractions brought about by the cysLTs. LTRAs prevent the binding of LTs to their receptors in the airways, thereby blocking bronchospasm. Zileuton is a 5-lipoxygenase (5-LO) pathway inhibitor. 5-LO is one of the pathways through which arachidonic acid can be metabolized to form LTs. The effect of both types of drugs is inhibition of the acute bronchoconstriction phase and inhibition of the delayed inflammatory phase of asthma. Bronchodilation with improved FEV1 and reduced markers of airway inflammation (particularly eosinophils) is the result. Leukotriene modifiers (LMs) may be used as an alternative to ICSs in patients with mild persistent or aspirin-sensitive asthma, but their effect is weaker than that of low-dose ICSs; therefore, they usually are used as add-on therapy in asthma. • Asthma is a chronic inflammatory disease of the airways that requires daily use of controller medication in most cases, even in young children. Only those with mild, intermittent asthma (symptoms ≤2 days per week or ≤2 nights per month) require no daily medication. They can be treated with as needed use of RABAs. • The preferred controller medication in adults and children with persistent asthma is low-dose ICS. An LM or a mast cell stabilizer may be considered as an alternative for long-term control. • The addition of a LABA for patients with moderate persistent asthma improves lung function and symptom control and reduces the need for quick relief medications. • Alternately, an LM, theophylline, or doubling the dose of ICS may be considered for add-on therapy in those 5 years of age and older. • For children younger than 5 with moderate persistent asthma, an increase to a medium-dose ICS given as monotherapy is followed by the addition of a LABA or LM. Treatment of severe persistent asthma requires high-dose ICS and a LABA or LM. • A course of oral corticosteroids may be used in severe asthma, but long-term steroid use should be avoided if possible. Specialists may consider omalizumab, a new monoclonal antibody directed against IgE that is the first biologic therapy targeted for use for the treatment of asthma, for severe asthma in those 12 years and older. • Quick relief medication (SABA is preferred) may be used at all stages of asthma for breakthrough symptoms or exacerbations. Ipratropium may be added for severe exacerbations. • Urgent medical care for exacerbations should include inhaled oxygen; adjunct therapy in refractory cases may include mechanical ventilation and heliox (inhaled helium and oxygen mixture). The NAEPP EPR3 guidelines (Figures 16-3 and 16-4) present a stepwise pharmacologic approach that corresponds to the severity of asthma in patients of all ages. Six steps replace a four-step approach from the EPR2 Guidelines. Therapy now varies slightly in the 0 to 4 age group, the 5 to 11 age group, and the 12 and older age group. Information is provided here for ages 5 and older. For stepwise therapy in the 0 to 4 age group, see the EPR2 Guideline website. The goals of therapy are to gain and maintain long-term control of asthma and to quickly and successfully treat asthma exacerbations. Control of asthma is defined as prevention of chronic and troublesome symptoms, maintenance of normal or near-normal pulmonary function, maintenance of normal exercise and activity levels, prevention of recurrent exacerbations, avoidance of adverse effects from drug therapy, and satisfaction of patient and family expectations for asthma care. • Step 1 therapy for adults and children 5 years and older with mild intermittent asthma involves a quick relief bronchodilator used intermittently with no long-term medication. Inhaled relatively selective β2-adrenergic agonist bronchodilators are preferred for all severities of asthma because of their minimal side effect profile. • Step 2 therapy requires a long-term antiinflammatory medication, in addition to a quick relief bronchodilator. Choices of long-term control medication include an ICS in low dose (preferred), a mast cell stabilizer, an LM, or possibly an oral theophylline. • Step 3 therapy distinguishes between the 5 to 11 and 12 and older age groups. For those 12 years and older, an ICS at medium dose as monotherapy or an ICS at low dose with the addition of a LABA is preferred therapy; alternative therapy is a low-dose ICS, given along with one of the following: a LABA, oral theophylline, or an LM. For those in the 5 to 11 age group, any of the therapies may be used without preference. • Step 4 therapy uses an ICS at medium dose along with a LABA (preferred); alternatively, medium-dose ICS plus LM or theophylline is given. • Step 5 therapy calls for high-dose ICS plus a LABA (preferred); alternatively, in the 5 to 11 age group, a high-dose ICS plus an LM or theophylline may be used. In the 12 and older age group, the biologic omalizumab may be added on for those who have allergies. • Step 6 therapy calls for high-dose ICS plus LABA plus an oral corticosteroid. A specialist may add omalizumab in the 12 and older age group; an LM or theophylline may be substituted for a LABA in the 5 to 11 age group.
Asthma and Chronic Obstructive Pulmonary Disease Medications
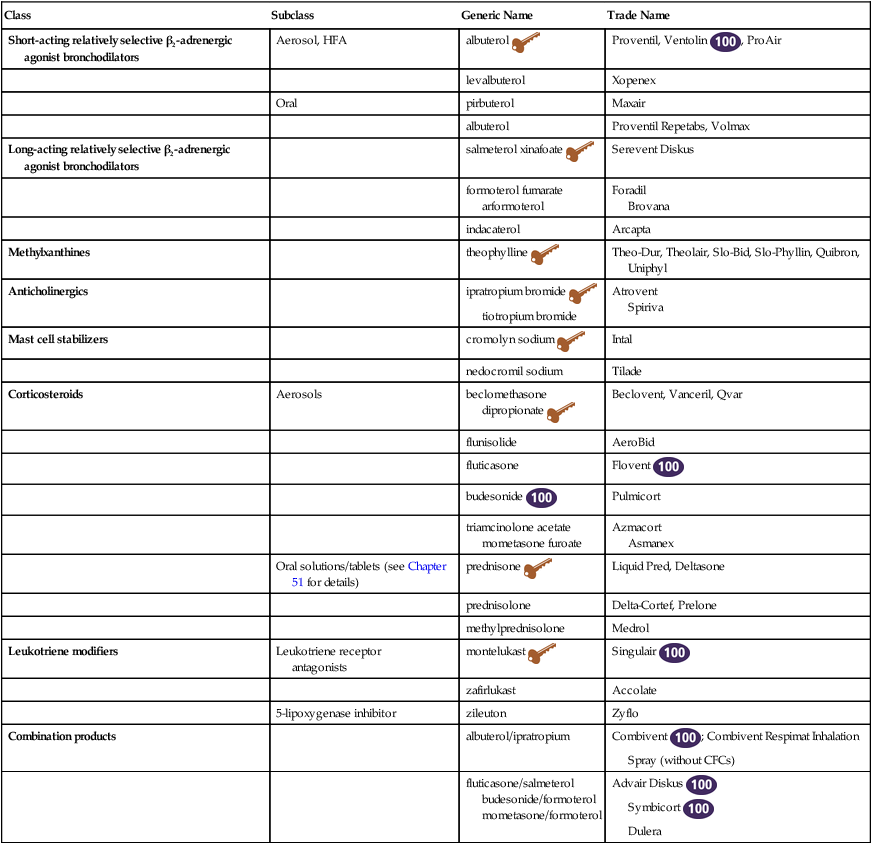
Class
Subclass
Generic Name
Trade Name
Short-acting relatively selective β2-adrenergic agonist bronchodilators
Aerosol, HFA
albuterol ![]()
Proventil, Ventolin ![]() , ProAir
, ProAir
levalbuterol
Xopenex
Oral
pirbuterol
Maxair
albuterol
Proventil Repetabs, Volmax
Long-acting relatively selective β2-adrenergic agonist bronchodilators
salmeterol xinafoate ![]()
Serevent Diskus
formoterol fumarate arformoterol
Foradil
Brovana
indacaterol
Arcapta
Methylxanthines
theophylline ![]()
Theo-Dur, Theolair, Slo-Bid, Slo-Phyllin, Quibron, Uniphyl
Anticholinergics
ipratropium bromide ![]()
tiotropium bromide
Atrovent
Spiriva
Mast cell stabilizers
cromolyn sodium ![]()
Intal
nedocromil sodium
Tilade
Corticosteroids
Aerosols
beclomethasone
dipropionate ![]()
Beclovent, Vanceril, Qvar
flunisolide
AeroBid
fluticasone
Flovent ![]()
budesonide ![]()
Pulmicort
triamcinolone acetate
mometasone furoate
Azmacort
Asmanex
Oral solutions/tablets (see Chapter 51 for details)
prednisone ![]()
Liquid Pred, Deltasone
prednisolone
Delta-Cortef, Prelone
methylprednisolone
Medrol
Leukotriene modifiers
Leukotriene receptor
antagonists
montelukast ![]()
Singulair ![]()
zafirlukast
Accolate
5-lipoxygenase inhibitor
zileuton
Zyflo
Combination products
albuterol/ipratropium
Combivent ![]() ; Combivent Respimat Inhalation Spray (without CFCs)
; Combivent Respimat Inhalation Spray (without CFCs)
fluticasone/salmeterol
budesonide/formoterol
mometasone/formoterol
Advair Diskus ![]()
Symbicort ![]()
Dulera
Therapeutic Overview of Asthma
Anatomy and Physiology
Location
Type
Example of Stimulus Response
Lung (smooth muscle)
α
Mild bronchoconstriction
β2
Bronchodilation; dilates arteries; relaxes alveolar walls
Mast cells
α
Augments release of histamine and other inflammatory mediators
β2
Inhibits release of inflammatory mediators
Heart
β1
Increases myocardial contraction, force, and velocity; stimulates glycogenolysis
Blood vessels
α
Vasoconstriction
β2
Vasodilation
Skeletal muscle
β2
Tremor; stimulates glycogenolysis
Multiple sites of action
α
Stimulates glycogenolysis; inhibits norepinephrine and acetylcholine release
β1
Stimulates lipolysis
β2
Stimulates norepinephrine release; inhibits acetylcholine release; moves potassium into cells; stimulates insulin release
Eyes (smooth muscle)
α
Mydriasis
Pathophysiology
Disease Process
Therapeutic Overview of Chronic Obstructive Pulmonary Disease
Anatomy and Physiology
Disease Process
Mechanism of Action
β-Adrenergic Agonist Bronchodilators
Corticosteroids
Leukotriene Modifiers
Treatment Principles of Asthma
Standardized Guidelines
Cardinal Points of Treatment
Pharmacologic Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree