http://evolve.elsevier.com/Edmunds/NP/
 Top 100 drug;
Top 100 drug;  key drug. Ibuprofen was chosen as the key drug because it was the first NSAID and is still in common use.
key drug. Ibuprofen was chosen as the key drug because it was the first NSAID and is still in common use.
Therapeutic Overview
In joints, the ends of the bones are capped by cartilage, and the joint structure is held together by a very tight capsule. A very fine membrane, the synovium, lines that capsule. The synovium normally stops at the point where the cartilage begins. The synovium does not extend across the whole joint; otherwise, trauma to the synovium would occur every time the joint was flexed (Figure 36-1). The tendons attach to the bones, and when the muscle contracts, the joint opens or closes.
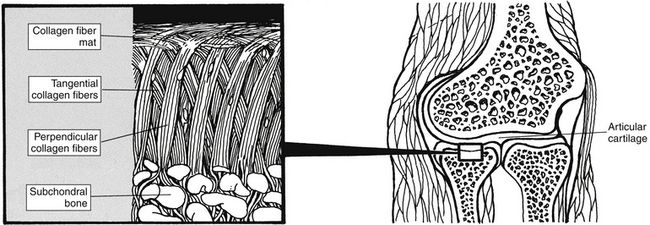
FIGURE 36-1 Organization of collagen fibers in articular cartilage. (From McCance KL, Huether SE: Pathophysiology, ed 4, St Louis, 2001, Mosby.)
Inflammation
See Chapter 70, Immunizations and Biologicals, for a review of the immune system. Prostaglandins cause increased vascular permeability and neutrophil chemotaxis (movement), and they induce pain. Increased vascular permeability allows diffusion of large molecule inflammatory substances across cell walls into the site of inflammation. Prostaglandins are produced in the mast cell from arachidonic acid by the action of the COX enzyme and are classified into groups according to their structure. Prostaglandins E1 and E2 are active in the inflammatory response. Aspirin and NSAIDs act to block the COX enzyme from producing prostaglandins, thereby inhibiting inflammation (Figure 36-2).
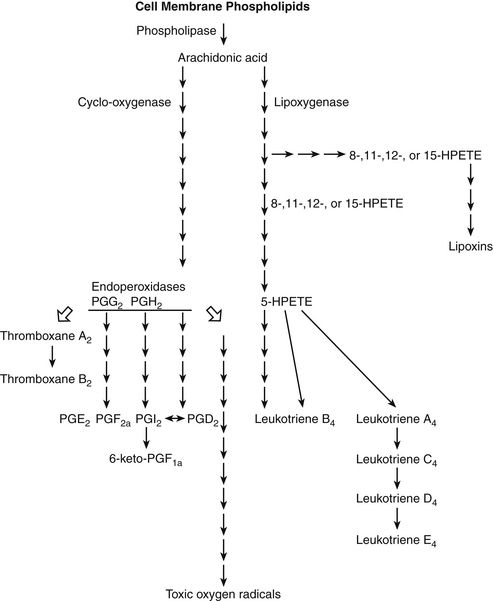
FIGURE 36-2 Arachidonic acid synthesis to prostaglandins. (Modified from Melmon K, Morrelli-Howard F: Clinical pharmacology: basic principles in therapeutics, ed 3, New York, 1992, McGraw-Hill.)
Two types of cyclooxygenase have been identified: COX-1 and COX-2. COX-1 is found in the blood vessels, stomach, and kidneys; COX-2 is found in the brain, kidneys, and bone. Inhibition of COX-2 is necessary to prevent inflammatory action.
COX-1 prostaglandins protect the gastric mucosa. They encourage mucosal blood flow and elaboration of bicarbonate to produce a more neutral or less acidic layer next to the gastric mucosa. Prostaglandins also produce a significant layer of mucus that serves as a barrier to the acid. They maintain normal renal function, mental function, and temperature. Although these effects are desirable, it is through COX-1 inhibition that salicylates and NSAIDs are thought to have their direct detrimental effects on the gastric mucosa. Selective COX-2 inhibitor drugs are designed primarily to inhibit COX-2 while sparing COX-1. Because this selectivity is not perfect, these drugs may exert some detrimental effect on the gastric mucosa. COX-1 drugs are widely available, but only one COX-2 drug is currently in use.
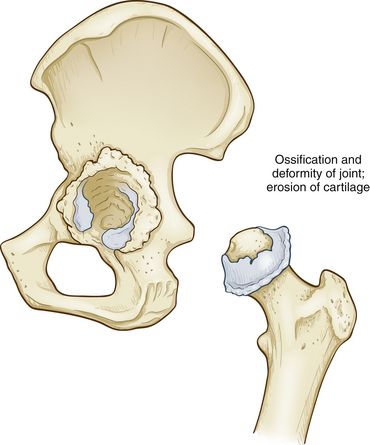
When an inflammatory process occurs, the synovium becomes lumpy. The synovium also starts to grow into and across the cartilaginous area, producing pits in the cartilage. At the same time, the tendon sheath that surrounds the tendon becomes inflamed, so motion of the joint is painful. If this process is not checked, ultimately, the ends of the bones are denuded and bone grates upon bone, with resultant eventual destruction of the joint (Figure 36-3). The inflammatory response is accompanied by symptoms of erythema, edema, tenderness, and pain.
Pathophysiology: Osteoarthritis
In OA, the articular cartilage degenerates, is roughened, and then is worn away. The body attempts to repair the lost cartilage, but the integrity of the new cartilage is inferior to that of the original, and the integrity of the surface of the cartilage is lost. Bone compensates by hypertrophy at the articular margins, forming spurs and causing lipping at the edge of the joint surface. The synovial membrane thickens, but it does not form adhesions. A low level of inflammation usually is present (see Figure 36-3).
Disease Process
More than 100 types of arthritis are known. The one thread that is common to all arthritic conditions is inflammation. Treating the inflammation is only one component of treating arthritis, but it is extremely important.
Characteristic symptoms of OA are pain with movement and weight bearing that is relieved by rest. The patient often has brief morning stiffness (less than 30 minutes) with minimal articular inflammation and no systemic manifestations. Joints commonly affected are terminal joints of the fingers, thumb, hip, knee, and spine. No signs of acute inflammation are seen, and the erythrocyte sedimentation rate is normal.
Mechanism of Action
Acetaminophen (APAP) is different from salicylates and NSAIDs in that it does not have significant antiinflammatory action. This is because APAP affects COX in the brain but not in peripheral tissue.
Salicylates and NSAIDs reduce inflammation by inhibiting the production of prostaglandins, prostacyclin, and thromboxanes in both CNS and peripheral tissue. They do this by blocking the COX enzyme. This major mechanism is involved in most of the effects achieved by salicylates and NSAIDs (see Figure 36-2) and may be responsible for the fact that the incidence of colon cancer has been found to be lower in patients who take ASA on a regular basis.
Pain
The mechanism for decreasing pain occurs through the antiinflammatory process. Pain is relieved when prostaglandin production is blocked, resulting in reduced inflammation. Salicylates may cause some pain reduction centrally at subcortical sites.
Antipyretic Effects
ASA blocks the effect of interleukin-1 on the hypothalamus, which is responsible for temperature control. Peripherally, salicylates reduce fever by causing vasodilation of superficial blood vessels. This effect results in dissipation of heat.
Platelet Effects
Platelet activation is stimulated by thromboxane; this results in aggregation, and the clotting cascade ensues. The antiplatelet effects of NSAIDs are caused by blocking of the COX-1 enzyme and production of thromboxane. Any drug that inhibits the COX-1 enzyme reduces the production of thromboxane. This effect is applied in the treatment of patients with cardiovascular disease. Aspirin causes irreversible inactivation of COX, allowing decreased production of thromboxane for the life of the platelet (8 to 10 days). NSAIDs, however, exhibit reversible inactivation of COX, which lasts only for the duration of drug activity, so continuous platelet aggregation is not found. This is why aspirin—not NSAIDs—is used for prevention of stroke and MI.
Ongoing research is examining the use of NSAIDs in the treatment of patients with a variety of problems:
Adverse Effects
When prostaglandins are inhibited, more gastric acid is produced and the risk of mucosal damage is increased. ASA and NSAIDs, by inhibiting prostaglandins, increase gastric acid production at the same time that they decrease defenses to that acid. This process serves as the basis for the adverse GI effects of these medications.
Kidneys that are impaired also rely on prostaglandins to cause vasodilation. When prostaglandins are inhibited, vasodilation is lessened and blood flow to the kidneys is decreased.
As with all NSAIDs, long-term use of celecoxib can lead to renal papillary necrosis, renal insufficiency, acute renal failure, and other renal injuries. In patients for whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion, NSAIDs may cause a dose-dependent reduction in prostaglandin formation and, secondarily, renal blood flow that may precipitate overt renal decompensation.
Patients with impaired renal function, heart failure, or liver dysfunction; elderly patients; and those taking diuretics, ACE inhibitors, and angiotensin II receptor antagonists are at greatest risk for this reaction. Discontinuation of NSAID therapy usually is followed by recovery to the pretreatment state.
A U.S. 2012 study about individuals with an initial heart attack found that those who took nonsteroidal anti-inflammatory drugs afterward seemed to have a greater risk of death or a repeat attack in the next five years. Researchers said 20% of NSAID users died during the first year after the heart attack, compared with about 12% of nonusers.
Treatment Principles
Evidence-Based Recommendations
For the person with moderate to severe pain and/or inflammation, a COX-2 selective NSAID is the first choice, unless the person is at significant risk for hypertension or renal disorder.
In persons at increased risk for hypertension and edema, clinicians should use any NSAID cautiously because of the risk of exacerbating hypertension or edema. Nonselective NSAIDs should be considered only if the person is not responsive to or is not able to take COX-2 selective NSAIDs and/or acetaminophen up to 4000 mg per day, and only after a risk analysis has been done to determine the risk for a significant NSAID-induced GI complication. If such risk factors exist, then a prophylactic agent such as a proton pump inhibitor or misoprostol should be given along with the nonselective NSAID.
The person at risk for a cardiovascular event should be given a regular low dose of aspirin (between 75 and 160 mg per day), whether the patient is treated with a nonselective or a COX-2 selective NSAID.
Tramadol may be used alone or in combination with acetaminophen or NSAIDs for therapy at any time during the treatment of a person with OA, when NSAIDs alone produce inadequate pain relief.
Cardinal Points of Treatment
Drug Choice
All NSAIDs differ from one another in terms of a number of drug properties. Evaluation of these properties in relationship to the patient and his or her condition will aid drug choice. Wide variation has been noted in how patients respond to a particular medication. As always, when many drugs are included in the same class, one should select a few and become familiar with them. Clinically, no clear guidelines and no evidence-based decision making are available to assist the provider in selecting the most appropriate NSAID for a particular patient.
Aspirin can be effective and inexpensive. Up to 12 tablets a day are required, so compliance can be difficult. Salicylates are generally less expensive than NSAIDs. Because salicylates almost always cause GI distress or ulceration, their use is significantly limited. U.S. researchers have found that aspirin intake reduces a person’s risk of developing Barrett’s esophagus, the top risk factor for esophageal cancer, by nearly 50%. The risk was lower in patients who took more than 325 milligrams of aspirin per day than those who took less.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 All of these drugs can cause GI irritation and bleeding, which can be fatal. GI bleeding may occur without any prodromal symptoms.
All of these drugs can cause GI irritation and bleeding, which can be fatal. GI bleeding may occur without any prodromal symptoms.
 A comprehensive review of the patient’s current drug regimen should be undertaken before salicylates or NSAIDs are added. Drug interactions with some products may increase the risk of untoward GI effects.
A comprehensive review of the patient’s current drug regimen should be undertaken before salicylates or NSAIDs are added. Drug interactions with some products may increase the risk of untoward GI effects.