USPSTF, United States Preventive Services Task Force.
Cancer Screening
- Cancer screening recommendations have been issued by many organizations, including the American Cancer Society (ACS; http://www.cancer.org, last accessed July 18, 2013), the National Cancer Institute (http://www.nci.nih.gov, last accessed July 18, 2013), the American College of Physicians (ACP; http://www.acponline.org, last accessed July 18, 2013), the United States Preventive Services Task Force (USPSTF; http://www.uspreventiveservicestaskforce.org/, last accessed July 18, 2013), and many specialty societies.
- As with screening for other conditions, the approach much be individualized.
CURRENT DISEASE MANAGEMENT
- The clinician should evaluate the status of chronic diseases and any potential new problems.
- Not every problem can be analyzed exhaustively at each visit.
- The average office visit is scheduled for approximately 15 minutes, so prioritization must occur and is usually based on the patient’s chief complaint and what the clinician feels is the most serious problem.
- Explanation of disease and relief of symptoms are keys to the patient’s satisfaction. Symptom relief does not always require prescription drug therapy but may include lifestyle changes, physical therapy, or over-the-counter medications.
- Reassurance that a symptom is not indicative of a more serious illness is important.
- Screening for risk factors and treating chronic conditions known to produce cardiovascular disease are critical components of ambulatory care.
Hypertension
High BP is the most common primary diagnosis in the United States and is often referred to as “the silent killer” because it is generally asymptomatic. See also Chapter 6.
- The relationship between BP and cardiovascular events is continuous, consistent, and independent of other risk factors.
- All adults should have their BP measured at least every 2 years, and more frequently if elevated, but the optimum screening interval is unknown.
- Persons should be seated quietly for at least 5 minutes in a chair, with feet on the floor and arm supported at heart level. At least two measurements should be made with an appropriate-sized cuff.
- Ambulatory BP monitoring provides more detailed information and can evaluate for “white coat” hypertension.
- Normal BP is <120/80.
- Prehypertension is defined by a systolic BP of 120 to 139 or a diastolic BP of 80 to 89 mm Hg. Prehypertensives are at high risk of developing hypertension, and early intervention can decrease the rate of progression to hypertension.
- A systolic BP >140 or diastolic BP of >90 mm Hg (measured on more than one reading) is considered hypertension. in patients younger than 65-years-old. For patients over age 65, the definition of hypertension is BP >150/90 mm Hg.
- Antihypertensive therapy has been associated with a 40% reduction in stroke, 25% reduction in myocardial infarction, and 50% reduction in heart failure.
- Initial therapy includes counseling on weight loss, aerobic exercise, limiting alcohol intake, and reduction of sodium intake. The decision as to whether to start drug therapy should depend on the severity of hypertension, the presence of other disease, and evidence of end organ damage.1
Dyslipidemia
Research from many different sources indicates that elevated LDL cholesterol is a major cause of coronary artery disease (CAD). See also Chapter 11.
- Cholesterol screening is recommended at least every 5 years for all adults older than 20 years of age.
- Screening is best performed with a lipid profile (total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides) obtained after a 12-hour fast.
- Individual patient risk assessment and classification is critical for determining treatment goals and therapeutic options.
- Initial therapy for patients with elevated cholesterol includes counseling to decrease consumption of fats and to promote weight loss in overweight patients.
- Clinical trials demonstrate that LDL-lowering therapy reduces risk for CAD.2,3
Diabetes Mellitus
- Diabetes mellitus (DM) requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications. See also Chapter 20.
- The American Diabetes Association standards of care are as follows:
- For decades, the diagnosis of DM was based on either fasting plasma glucose (FPG) or the 2-hour oral glucose tolerance test (OGTT).
- In 2009, an international expert committee recommended the use of the A1C test to diagnose DM, with a threshold of ≥6.5%.
- The established glucose criteria for the diagnosis of DM remain valid. FPG ≥126 mg/dL, 2-hour plasma glucose ≥200 mg/dL during an OGTT, and a random plasma glucose ≥200 mg/dL with classic symptoms of hyperglycemia or hyperglycemic crisis are all diagnostic.
- For decades, the diagnosis of DM was based on either fasting plasma glucose (FPG) or the 2-hour oral glucose tolerance test (OGTT).
- Asymptomatic adults with sustained BP (treated or untreated) >135/80 mm Hg should be screened for diabetes.
- Screen overweight (body mass index [BMI] ≥25 kg/m2) adults who have additional risk factors (presented in Table 1-2).
- Patients with prediabetes should be referred to an effective ongoing support program targeting weight loss and increasing physical activity.4
Table 1-2 Criteria for Testing for DM in Asymptomatic Adults
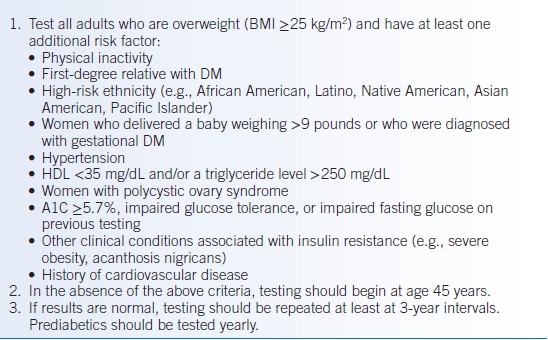
Modified from American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care 2012;35:S11–S63.
Obesity
- Periodic height and weight measurements are recommended for all patients. See also Chapter 22.
- The BMI is calculated as weight in kilograms divided by the height in meters squared.
- BMI ≥25 kg/m2 is considered overweight.
- BMI ≥30 kg/m2 is considered obese.
- BMI ≥40 kg/m2 is considered severely obese.
- BMI ≥25 kg/m2 is considered overweight.
- More than one-third of US adults are obese.
- Obesity increases the risk of many health conditions including heart disease, stroke, diabetes, and certain cancers.
- Diet and exercise are the cornerstones of weight loss, though medications and bariatric surgery can be considered when lifestyle changes fail.5
Tobacco Abuse
- An estimated 45.3 million (19.3%) US adults smoke cigarettes. See also Chapter 45.6
- Cigarette smoking is the leading cause of preventable death in the United States, accounting for one of every five deaths each year.
- Although only approximately 7% of patients are able to quit long term on their own, it is estimated that counseling and appropriate pharmacotherapy can increase the quit rate to 15% to 30%.
- A widely accepted approach to brief office-based counseling and pharmacotherapy was published by the U.S. Public Health Service in 2008.7

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


