Applied Anatomy of the Chest Wall and Mediastinum
Petros Mirilas
Michael E. Halkos
John D. Symbas
Panagiotis N. Symbas
Lee J. Skandalakis
Chest Wall
Embryogenesis
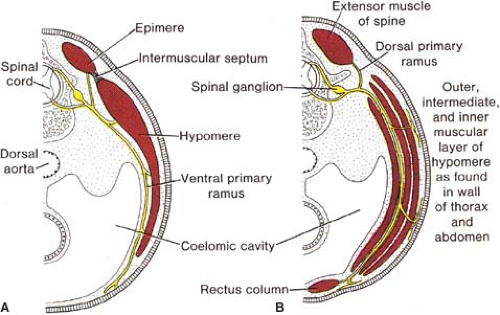
The muscles of the chest develop from the somites found in the mesoderm. About the 6th week, the somites differentiate into the sclerotomes and the dermatomyotomes. The myotomes elongate and invade the mesoderm of the wall of the embryonic thoracic and abdominal cavities. These myotomes divide into the epimere and the hypomere. The corresponding nerves give a dorsal and a ventral ramus, respectively. The hypomere in turn divides in three layers—outer, intermediate, and inner—that give the three layers of muscles of the chest, that is, the external intercostals, the internal intercostals, and the innermost intercostals; in the abdomen, the hypomere gives off the external oblique, the internal oblique, and the transverse abdominal muscles (Fig. 1). This arrangement explains the continuity of the three muscle layers in the thoracic and abdominal wall. The anterior edge of the hypomere gives the rectus abdominis, and, in the thoracic wall, its equivalent: the transverse thoracic muscle.
The ribs develop in the 5th week by the costal processes of the thoracic vertebrae (derivatives of the sclerotomes). They elongate in the same mesodermal layer with the thoracic muscles, and thus the investing fasciae of the intercostal muscles are continuous with the periosteum of the ribs. The embryonic ribs are cartilaginous; ossification takes place about the 9th week.
The sternum appears during the 6th week as paired bands of condensed mesenchyme. At the same time, the presternum, a cranial rudiment associated with the development of the shoulder, and two craniolateral pieces, the suprasternal cartilages, will join the two sternal bars, which “zipper” craniocaudally (Fig. 2). The manubrium is the result of subsequent ossification in the sternum.
Congenital Anomalies
Sternum deformities (Fig. 3): The pectus excavatum or funnel chest represents a depression deformity, with the apex at the lower end of the body of the sternum. The pectus carinatum or pigeon breast is a protrusion deformity. These deformities are often nonsymmetrical or mixed. Sternal clefts (upper, lower, or entire) may be the outcome of an anomaly of fusion of the two sternal bars; this deformity may be associated with ectopia cordis (cardiac ectopia), or, rarely, may be one of the constituents of Cantrell’s pentalogy (sternal cleft, diaphragmatic defect, defect of the pericardium and communication with abdomen, cardiac defects).
Rib deformities: The spectrum of these rare anomalies includes unilateral absence, absence of cartilage, separation of cartilage and rib, combined costosternal anomalies, and part of a skeletal disorder combined with the absence of the pectoralis major muscle (Poland’s syndrome).
Surface Anatomy
Sternum
Parts of the sternum point to the position of deep structures:
The superior border lies in the same horizontal level as the inferior border of the body of the second thoracic vertebra. McGregor and Du Plessis wrote about this border:
A pin pushed back at the middle of the upper border of the sternum would transfix the inner border of the innominate artery just below its division. In the child the top of the aortic arch may reach the upper border of the manubrium, whereas in the adult it is about the level of the center of this bone.
The angle of Ludwig or of Louis, that is, the junction of the manubrium with the body of the sternum, lies on the same horizontal level with the fourth thoracic vertebra, the bifurcation of the aorta (one vertebra higher in the infant), the beginning and the end of the aortic arch, the site where the pleural sacs meet. The angle of Louis is useful for counting the ribs, because the second rib lies opposite to it.
The xiphisternal junction lies at the level of the disk between 9th and 10th thoracic vertebra.
Lung and Pleura Projection
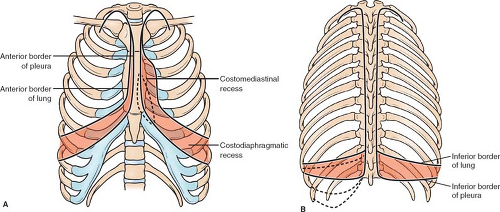
The classical teaching is that the inferior border of the lungs (defined by percussion) begins at the xiphisternal junction, then is found at the 6th rib in the midclavicular line, the 8th in the midaxillary line, and the 10th vertebra at the spine. The pleura is supposed to be found two spaces below at all these points; an empty costodiaphragmatic recess lies in between (Fig. 4). However, as O’Rahilly points out, it is not empty but occupied by a very thin part of the lung, which expands further in deep inspiration. Surgically, we must consider that the lung and pleura coexist. It is also important to know the exact levels of the costomediastinal sinuses (Fig. 4A) to gain transthoracic access to the pericardium, heart, and esophagus without producing pneumothorax; for example, the pericardium can be reached through the fifth and sixth interspaces without opening the pleura. Another must-know tip is the extension of the cervical pleura into the neck: the cupola of the pleura lies behind the sternocleidomastoid muscle, 2 to 3 cm or more above the medial third of the clavicle. This space is filled by lung. The subclavian artery, the internal thoracic vessels, the inferior ganglion of the cervical chain, the lower trunk of the cervical plexus all lie on the cervical pleura.
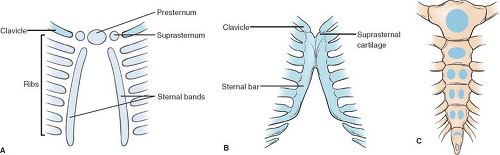 Fig. 2. Development of the sternum. A: Mesenchymal stage (6th week). B: Cartilaginous stage (9th week). C: Ossification centers appearing after birth. |
The lung, pleura, liver, stomach, spleen, colon, kidney, and peritoneal cavity extend higher to the periphery of the diaphragm and the inferior border of the lungs. A perforating trauma to the lower intercostals must be considered and treated as thoracoabdominal trauma.
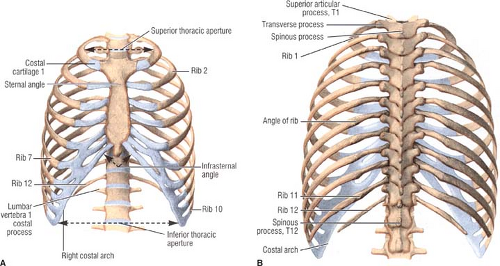
Bony Thorax
The thoracic cage includes the sternum, the ribs, and the vertebrae (Fig. 5). The sternum consists of the manubrium, the body, and the xiphoid process. The first seven pairs of ribs are the true ribs, and the last five the false ribs; of the last, ribs 8 to 10 articulate with the sternum via supervening costal cartilages, while ribs 11 and 12 do not articulate at all (floating ribs). Occasionally, the 12th rib is missing; a cervical rib is encountered in 1%, producing symptoms only in 10% of these.
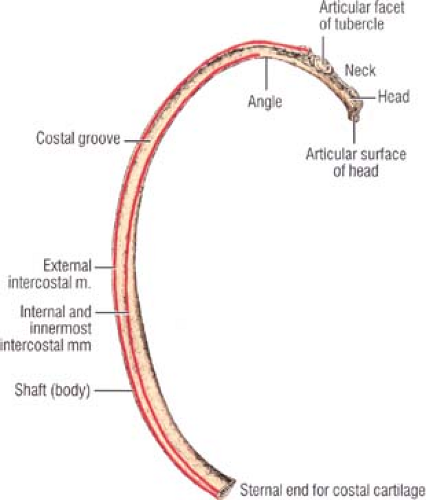
A typical rib (Fig. 6) has a head, with superior and inferior articulation facets with the superior and inferior vertebra, respectively; a neck; an angle; and the shaft. The costal groove is located in the inferior internal surface of the rib and hosts the neurovascular intercostal bundle. Fracture of the rib due to compression is unusual, and happens at the apex of the curve, sparing the pleura. Otherwise, with direct injury, the fractured rib may traumatize the pleura, the lung, and the intercostal vessels, leading to pneumothorax, hemothorax, or even subcutaneous emphysema.
Muscles
Extrinsic Muscles
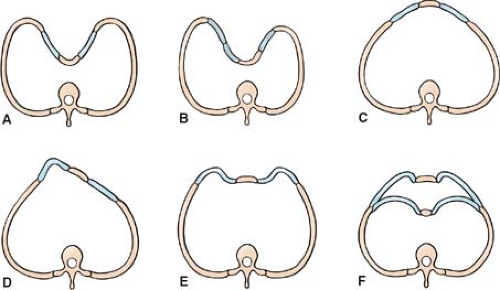 Fig. 3. Varieties of chest deformities (in cross section). A,B: Depression deformities. C,D: Protrusion deformities. E: Bilateral protrusion. F: Chondromanubrial protrusion with gladiolar depression. |
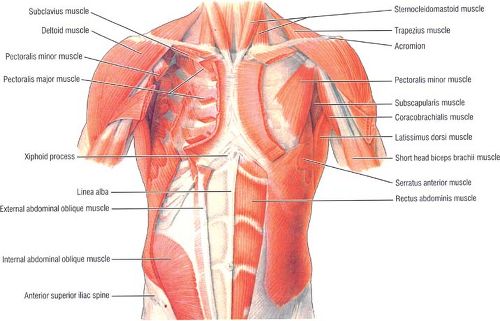
The thoracic cage is to a great extent covered by muscles that do not belong to the thorax, but to the shoulder, neck, back, or abdominal wall. The pectoralis muscles,
major (lateral and medial pectoral nerve, C5 to C7) and minor, and the serratus anterior (long thoracic nerve) are the extrinsic muscles of the anterior and lateral chest wall (Fig. 7). The muscles of the anterior abdominal wall cover the lower ribs: the external oblique from the eight lower ribs (its slips interdigitate with the serratus anterior), the internal oblique (which attaches to the lower three ribs), the internal oblique from the inner surfaces of the eight lower costal cartilages, and the rectus abdominis (which inserts in front of the xiphoid process and into the fifth to seventh costal cartilages).
major (lateral and medial pectoral nerve, C5 to C7) and minor, and the serratus anterior (long thoracic nerve) are the extrinsic muscles of the anterior and lateral chest wall (Fig. 7). The muscles of the anterior abdominal wall cover the lower ribs: the external oblique from the eight lower ribs (its slips interdigitate with the serratus anterior), the internal oblique (which attaches to the lower three ribs), the internal oblique from the inner surfaces of the eight lower costal cartilages, and the rectus abdominis (which inserts in front of the xiphoid process and into the fifth to seventh costal cartilages).
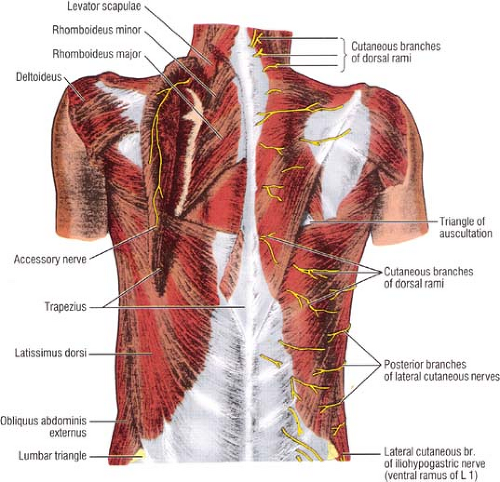
The extrinsic muscles of the posterior thoracic wall are the trapezius (spinal accessory nerve, XI), the latissimus dorsi
(thoracodorsal nerve), the serratus posterior superior and inferior (segmental rami), the rhomboids, and the levator scapulae (Fig. 8).
(thoracodorsal nerve), the serratus posterior superior and inferior (segmental rami), the rhomboids, and the levator scapulae (Fig. 8).
Intrinsic Muscles
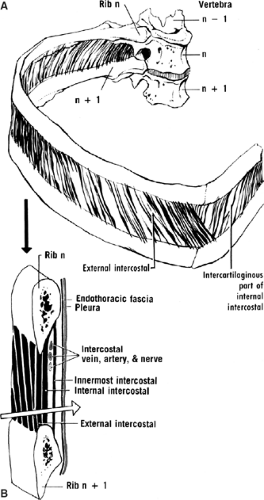
Similar to the abdominal wall, the thoracic wall includes three muscle layers (Fig. 9). The neurovascular bundle lies between the middle and internal layer.
The superficial layer consists of the external intercostal muscles. Their direction is downward and forward, similar to the external oblique abdominal muscle, with which the lower seven are continuous. They extend from the tubercle of the rib to the costochondral junction, where they are replaced by the homonymous membrane.
The middle layer comprises the internal intercostal muscles. They extend from the medial ends of the ribs anteriorly to the angle of the ribs posteriorly, where they are replaced by the homonymous membrane.
The internal layer is noncontinuous around the inner surface of the chest wall and comprises the innermost intercostals, the subcostals, and the transversus thoracis.
No fat is found between the endothoracic fascia (covering the internal surface of the internal muscle layer) and the pleura. In contrast, in the abdominal wall, preperitoneal fat is found between the endoabdominal fascia and the peritoneum.
Vessels
Arteries
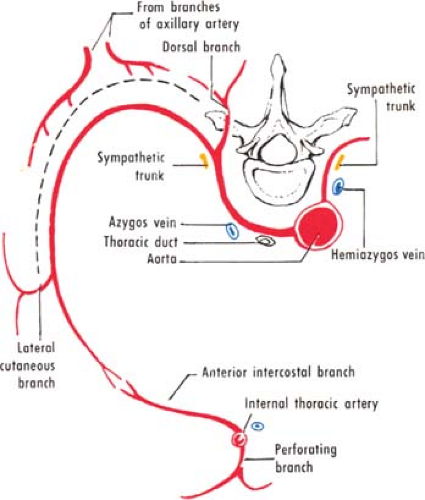
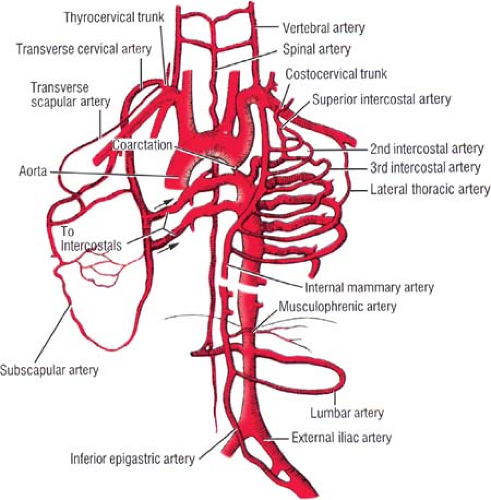
The vascular supply of the chest wall is rich and originates from different sources. The chest wall is supplied by the posterior intercostal arteries arising from the aorta, the internal thoracic and the highest intercostals given off the subclavian artery, and the branches of the axillary artery (Fig. 10). Surgical mastery of this two-source arterial network (aorta-subclavian, and axillary arteries) can be reached if the surgeon studies the collateral circulation developing in aortic coarctation (Fig. 11).
The principal arteries are the (posterior) intercostals and the internal thoracic arteries. The first two or three pairs of the intercostal arteries arise from the highest intercostal artery, a branch of the costovertebral trunk of the subclavian artery. The remaining intercostal arteries are given from the back of the aorta. The right arteries pass in front of the vertebrae, and hence are longer than the left. The intercostal arteries lie behind the azygos and hemiazygos veins, the thoracic duct, and the sympathetic trunk (Fig. 10). The arteries course in the costal groove between the vein (above) and the nerve (below). This is true for the dorsal and lateral chest; anteriorly, vessels and nerve are exposed in the spaces. Therefore, in the dorsal and lateral chest, the surgeon must proceed along the superior margin of the lower rib when puncturing in order to aspirate or to perform surgical procedures. This relation with the bone explains the risk for vessel wound in rib fractures.
The intercostal artery gives off branches. One is the dorsal artery, muscular and spinal, which supplies the muscles and skin of the back. Another branch is the lateral cutaneous for the overlying muscles; the third to fifth give small mammary branches. In most cases the intercostal artery, at the angle of the rib, gives off a collateral artery, which then travels anteriorly immediately above the lower rib. This vessel is much smaller than the main one. It is not unusual to disregard the presence of this vessel during paracentesis through a posterolateral part of an intercostal space; inserting the needle at the upper border of the lower rib to avoid the main intercostal artery and nerve can traumatize the collateral.
The internal thoracic artery arises from the first part of the subclavian artery (Fig. 12). It courses downward in the thorax just lateral to the sternum, behind the upper six costal cartilages and the internal intercostal muscles, and in front of the transverse thoracic muscle and the pleura. In the sixth space the internal thoracic artery divides into a lateral branch (the musculophrenic artery) and a terminal branch, feeding the rectus muscle (the superior epigastric artery). The rectus can be used in reconstruction of the breast as a flap reversed upward around the superior epigastric artery. Other branches are the anterior intercostals arteries and the perforating arteries in the upper six spaces; the latter in the second to fourth spaces supply the breast. The internal thoracic artery can be ligated—for example, in case of trauma resulting in a possibly fatal hemorrhage—in the third intercostal space; lower spaces are much narrower for this procedure.
The anterior intercostal arteries are sometimes two (inferior and superior) in the respective intercostal space; sometimes
the lower, traveling on the upper border of the lower rib, is the bigger. To perform paracentesis through an anterior intercostal space, the surgeon is advised to proceed in the middle of the space to avoid bleeding from the anterior intercostal arteries.
the lower, traveling on the upper border of the lower rib, is the bigger. To perform paracentesis through an anterior intercostal space, the surgeon is advised to proceed in the middle of the space to avoid bleeding from the anterior intercostal arteries.
Veins
The posterior intercostal veins and the subcostal veins follow the posterior intercostal arteries in the costal grooves. The 1st posterior intercostal vein on either side empties into the brachiocephalic vein. The 2nd through 4th veins join the superior intercostal vein, which on the right joins the azygos vein and on the left the left brachiocephalic vein. The left superior intercostal lies next to the aorta and can be mistaken for aortic aneurysm. The rest of the intercostal veins (5th to 12th) empty into the azygos (right side) or into the hemiazygos and accessory hemiazygos on the left side (Fig. 13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree