EXAMINATION
Have patient in knee-chest or left lateral position with hips and knees flexed, or standing with hips flexed and upper body supported by examining table. Drape patient appropriately.
| TECHNIQUE | FINDINGS |
|---|---|
| Wear gloves on both hands | |
| Inspect and palpate sacrococcygeal and perianal area | |
 Skin characteristics Skin characteristics | EXPECTED:Smooth and uninterrupted. |
| UNEXPECTED:Lumps, rashes, tenderness, inflammation, excoriation, pilonidal dimpling, or tufts of hair. | |
| Inspect anus | |
 Skin characteristics Skin characteristics | EXPECTED:Skin coarser and darker than on buttocks. |
| UNEXPECTED:Skin lesions, skin tags or warts, external or internal hemorrhoids, fissures and fistulas, rectal prolapse, or polyps. Describe any irregularities and locate using clock referents (12 o’clock ventral midline/6 o’clock dorsal midline). | |
| Inspect, palpate, assess sphincter tone | |
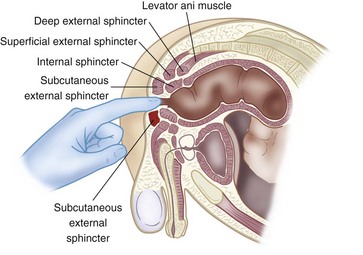
| Put water-soluble lubricant on index or middle finger; press pad against anal opening, and ask patient to bear down to relax external sphincter. As relaxation occurs, slip tip of finger into anal canal, as shown in figure below. (Assure patient that although he or she may feel the urgency of a bowel movement, it will not occur.) Ask patient to tighten external sphincter around finger. | EXPECTED:Even sphincter tightening. |
| UNEXPECTED:Patient discomfort. Lax or extremely tight sphincter, tenderness. | |
 | |
| Palpate muscular anal ring | |
| Rotate finger. | EXPECTED:Smooth, even with consistent pressure exerted. |
| UNEXPECTED:Nodules or other irregularities. | |
| Palpate lateral and posterior rectal walls | |
| Insert finger farther, and rotate to palpate lateral, then posterior, rectal walls. (If helpful, perform bidigital palpation with thumb and finger by lightly pressing thumb against perianal tissue and bringing finger toward thumb.) | EXPECTED:Smooth, even, uninterrupted. |
| UNEXPECTED:Nodules, masses, polyps, tenderness, or irregularities. (Internal hemorrhoids not ordinarily felt unless thrombosed.) | |
| Males: Palpate posterior surface of prostate gland through anterior rectal wall | |
| Rotate finger and palpate anterior rectal wall and posterior surface of prostate gland. (Alert patient that he may feel urge to urinate but will not.) | |
 Consistency and characteristics of anterior rectal wall Consistency and characteristics of anterior rectal wall | EXPECTED:Smooth, even, uninterrupted. |
| UNEXPECTED:Nodules, masses, polyps, tenderness, or irregularities. | |
 Consistency, contour, characteristics of prostate Consistency, contour, characteristics of prostate | EXPECTED:Surface firm and smooth, lateral lobes symmetric, median sulcus palpable, seminal vesicles not palpable. |
| UNEXPECTED:Rubberiness, bogginess, fluctuant softness, stony hard nodularity, tenderness, obliterated sulcus, or palpable seminal vesicles. | |
 Mobility of prostate gland Mobility of prostate gland | EXPECTED: Slightly movable. |
 Size of prostate gland Size of prostate gland | EXPECTED:4 cm diameter with less than 1 cm protruding into rectum. |
| UNEXPECTED:Protrusion greater than 1 cm (note distance of protrusion). | |
| UNEXPECTED:Discharge that appears at urethral meatus (collect specimen for microscopic examination). | |
| Females: Palpate uterus through anterior rectal wall | |
| Attempt to palpate uterus and cervix through anterior rectal wall. | |
 Position Position | EXPECTED:Midline, retroflexed or retroverted. |
| UNEXPECTED:Deviation to right or left. | |
 Surface characteristics Surface characteristics | EXPECTED:Smooth. |
| UNEXPECTED:Irregular. | |
| Have patient bear down, and palpate deeper | |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |



