Chapter 24 James D. Hoehns and Dana J. McDougall A variety of lipid disorders can occur as a primary event or an event that is related to some underlying disease. Dyslipidemia can result from genetic disorders, concomitant disease states, or environmental factors. Alterations in lipoprotein metabolism are complex and often multifactorial. The primary dyslipidemias are associated with overproduction or impaired removal of lipoproteins. Primary dyslipidemias and their associated abnormalities are listed in Table 24-1. Often, the cause of primary dyslipidemia is not identified and plays little or no role in the diagnosis and treatment of most patients. TABLE 24-1 Primary Dyslipidemia and Associated Abnormalities Table 24-2 provides a list of causes that contribute to secondary hyperlipidemia. If the clinician determines that a patient’s hyperlipidemia may be related to another process, correction or modification of this process should be sought before pharmacologic treatment is provided for the hyperlipidemia. Not mentioned in Table 24-2 is obesity, which may also produce lipoprotein alterations. In diabetes, triglyceride levels are related to the degree of glycemic control. In hypothyroidism, lipid abnormalities are corrected with thyroxine replacement. In uremia, an elevated triglyceride and low HDL level is observed. Elevated total cholesterol and triglycerides are seen in patients with nephrotic syndrome. In drug-induced hyperlipidemia, estrogens may increase HDL, whereas β-blockers, progestins, and anabolic steroids may decrease HDL. TABLE 24-2 Disorders Associated with Secondary Hyperlipoproteinemia This chapter incorporates the updated Adult Treatment Panel (ATP) III guidelines for the treatment of hyperlipidemia from the National Cholesterol Education Program (NCEP, 2004). (See http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm.) Other useful hyperlipidemia guidelines from the American Association of Clinical Endocrinologists can be found at http://www.aace.com/pub/guidelines/. (New guidelines will be announced in 2013.) USDHHS Expert Panel, Integrated Guidelines for the Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart Lung and Blood Institute: http://www.nhlbi.nih.gov/guidelines/cvd_ped/index.htm. • Decreased LDL level is the primary target of cholesterol-lowering therapy. • Statins are the preferred initial treatment choice and should be used at a dosage sufficient to lower LDL by 30%-40% in most patients. • Patients with diabetes (viewed as a CHD equivalent), coronary heart disease, or a 10-year risk of developing coronary heart disease >20% (calculated via Framingham risk scoring) have a goal LDL of <100 mg/dl (with an optional goal of <70 mg/dl if deemed “very high risk”). • If maximal dose statin is unable to achieve goal LDL, then statin + ezetimibe or statin + bile acid sequestrant may be useful combinations to lower this marker (which serves as a surrogate for risk). • If triglycerides are 200 to 499 mg/dl after the LDL goal has been reached, consider adding a niacin or fibrate (gemfibrozil or fenofibrate). Of the fibrates, fenofibrate is safer to use concomitantly with a statin. • If triglycerides are ≥500 mg/dl, the first goal is to lower triglycerides to prevent pancreatitis. Fibrates are typically the first choice. • If HDL is low (<40 mg/dl) after LDL goal is reached, consider adding niacin or a fibrate in patients with CHD or CHD equivalent. The most widely recognized treatment guidelines for hyperlipidemia, those of the NCEP, were most recently updated in 2004, although it is anticipated that another update will be released in 2013. An important tenet of these guidelines is that the intensity of evaluation and treatment depends on the patient’s overall risk status for CHD (Box 24-1)—that is, those patients with preexisting CHD or with CHD risk equivalents or those who are at high risk (more than two risk factors) for CHD in the near future are treated more aggressively. Next, patients with two or more risk factors should be further classified into 10-year risk groups based on their Framingham point scores. (See Framingham tables at www.nhlbi.nih.gov/guidelines/cholesterol/risk.) Framingham scores are based on age, total cholesterol level, smoking status, HDL cholesterol, and systolic blood pressure. They are used to assess the individual’s 10-year risk of developing CHD. Three levels of 10-year risk are identified: >20%, 10% to 20%, and <10%. Those found to have a risk >20% are categorized as if they had a CHD risk equivalent (for further information, see NCEP guidelines). A second important feature of the NCEP guidelines is that dietary and drug treatment decisions are based on LDL cholesterol levels (Table 24-3). For example, an individual whose blood pressure is 150/95 mm Hg who currently smokes and has a 10-year risk of 8% would have lifestyle changes initiated at an LDL level 130 mg/dl. According to the recommendations, this individual would initiate drug therapy with an LDL level ≥160 mg/dl. In contrast, an individual with the risk factors listed earlier and a 10-year risk of 12% would initiate therapeutic lifestyle changes and drug therapy at an LDL ≥130 mg/dl. Alternatively, the current guidelines would consider drug therapy “optional” for LDL values between 100 and 129 mg/dl in such an individual. TABLE 24-3 Treatment Decisions Based on LDL Cholesterol Levels ∗Non-HDL cholesterol is equal to total cholesterol − HDL cholesterol. Although achieving the goal LDL value is the first and primary goal, triglycerides and HDL should be considered in drug selection (Table 24-4). If triglycerides are >200 mg/dl after the LDL goal is reached, NCEP recommends setting a goal for non-HDL cholesterol (total cholesterol − HDL cholesterol) that is 30 mg/dl higher than the LDL goal. Once the LDL goal has been reached and triglycerides are <200 mg/dl, the focus should turn to the patient’s HDL. The first step in treatment is to increase physical activity and lose weight if overweight. Drug therapy, nicotinic acid, or fibric acid derivatives may be used if the patient’s HDL level remains below 40 mg/dl. TABLE 24-4
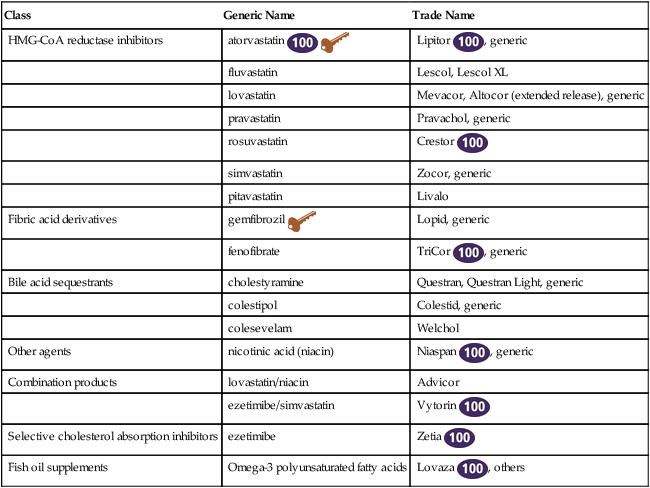
Antihyperlipidemic Agents
Class
Generic Name
Trade Name
HMG-CoA reductase inhibitors
atorvastatin ![]()
![]()
Lipitor ![]() , generic
, generic
fluvastatin
Lescol, Lescol XL
lovastatin
Mevacor, Altocor (extended release), generic
pravastatin
Pravachol, generic
rosuvastatin
Crestor ![]()
simvastatin
Zocor, generic
pitavastatin
Livalo
Fibric acid derivatives
gemfibrozil ![]()
Lopid, generic
fenofibrate
TriCor ![]() , generic
, generic
Bile acid sequestrants
cholestyramine
Questran, Questran Light, generic
colestipol
Colestid, generic
colesevelam
Welchol
Other agents
nicotinic acid (niacin)
Niaspan ![]() , generic
, generic
Combination products
lovastatin/niacin
Advicor
ezetimibe/simvastatin
Vytorin ![]()
Selective cholesterol absorption inhibitors
ezetimibe
Zetia ![]()
Fish oil supplements
Omega-3 polyunsaturated fatty acids
Lovaza ![]() , others
, others
Therapeutic Overview
Anatomy and Physiology
Pathophysiology
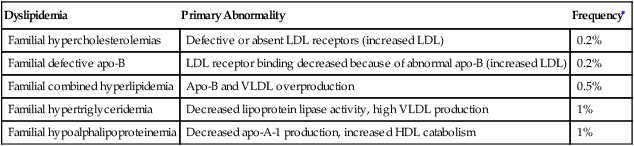
Dyslipidemia
Primary Abnormality
Frequency∗
Familial hypercholesterolemias
Defective or absent LDL receptors (increased LDL)
0.2%
Familial defective apo-B
LDL receptor binding decreased because of abnormal apo-B (increased LDL)
0.2%
Familial combined hyperlipidemia
Apo-B and VLDL overproduction
0.5%
Familial hypertriglyceridemia
Decreased lipoprotein lipase activity, high VLDL production
1%
Familial hypoalphalipoproteinemia
Decreased apo-A-1 production, increased HDL catabolism
1%
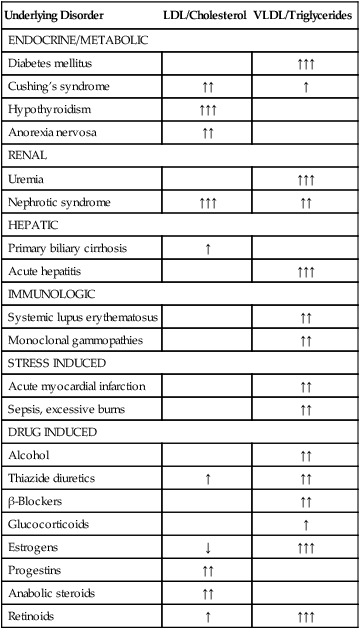
Underlying Disorder
LDL/Cholesterol
VLDL/Triglycerides
ENDOCRINE/METABOLIC
Diabetes mellitus
↑↑↑
Cushing’s syndrome
↑↑
↑
Hypothyroidism
↑↑↑
Anorexia nervosa
↑↑
RENAL
Uremia
↑↑↑
Nephrotic syndrome
↑↑↑
↑↑
HEPATIC
Primary biliary cirrhosis
↑
Acute hepatitis
↑↑↑
IMMUNOLOGIC
Systemic lupus erythematosus
↑↑
Monoclonal gammopathies
↑↑
STRESS INDUCED
Acute myocardial infarction
↑↑
Sepsis, excessive burns
↑↑
DRUG INDUCED
Alcohol
↑↑
Thiazide diuretics
↑
↑↑
β-Blockers
↑↑
Glucocorticoids
↑
Estrogens
↓
↑↑↑
Progestins
↑↑
Anabolic steroids
↑↑
Retinoids
↑
↑↑↑
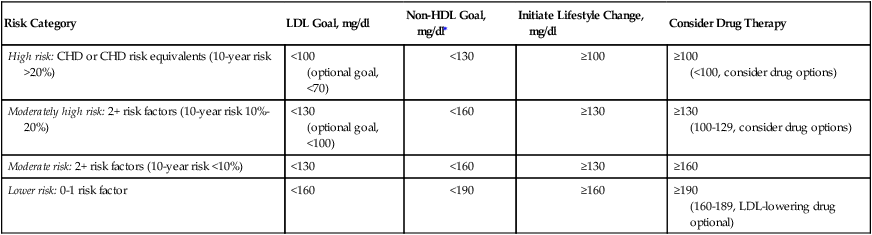
Treatment Principles
Standardized Guidelines
Cardinal Points of Treatment
Risk Category
LDL Goal, mg/dl
Non-HDL Goal, mg/dl∗
Initiate Lifestyle Change, mg/dl
Consider Drug Therapy
High risk: CHD or CHD risk equivalents (10-year risk >20%)
<100
(optional goal, <70)
<130
≥100
≥100
(<100, consider drug options)
Moderately high risk: 2+ risk factors (10-year risk 10%-20%)
<130
(optional goal, <100)
<160
≥130
≥130
(100-129, consider drug options)
Moderate risk: 2+ risk factors (10-year risk <10%)
<130
<160
≥130
≥160
Lower risk: 0-1 risk factor
<160
<190
≥160
≥190
(160-189, LDL-lowering drug optional)
Pharmacologic Treatment
Drug
LDL, %
HDL, %
TG, %
Bile acid sequestrants
↓15-30
↑0-3
No change
niacin
↓10-25
↑15-35
↓25-30
HMG-CoA inhibitors
↓20-60
↑5-10
↓10-30
gemfibrozil
↓10-15
↑15-25
↓35-50
fenofibrate
↓6-20
↑18-33
↓40-50
ezetimibe
↓15-18
↑2-4
↓4-6
Fish oil supplements
↑17-30
↑6-13
↓40-50 ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antihyperlipidemic Agents
Only gold members can continue reading. Log In or Register to continue
