2. Slightly cephalad to the vomiting center is the chemoreceptor trigger zone (CRTZ), which detects noxious chemicals in the bloodstream (ethanol at high concentration).
V. Prophylaxis. Antiemetic agents should be used for the prevention and treatment of nausea and vomiting when indicated but not routinely. In order to determine whether prophylaxis is indicated, it is important to assess a patient’s propensity to develop PONV according to risk factors that increase or decrease a patient’s chances of experiencing PONV.
A. Patient Factors. Women, nonsmokers, and those with a history of motion sickness or of previous episodes of PONV are at an increased risk of experiencing PONV.
B. Surgical Factors
1. The longer the surgical procedure, the greater is the risk for a patient to develop PONV.
2. Independent of duration, certain surgical procedures have been associated with an increased incidence of PONV (gynecologic surgeries; laparoscopic procedures; ear, nose, and throat; breast; plastic; and orthopedic surgical procedures).
3. Among adults, risk is reduced with aging.
C. Anesthetic Factors. Inhalation anesthetic agents nitrous oxide, neostigmine, and opioids have all been implicated in the genesis of PONV (correlation is limited and most scoring systems used to identify patients at risk of PONV do not use anesthetic factors as risk factors).
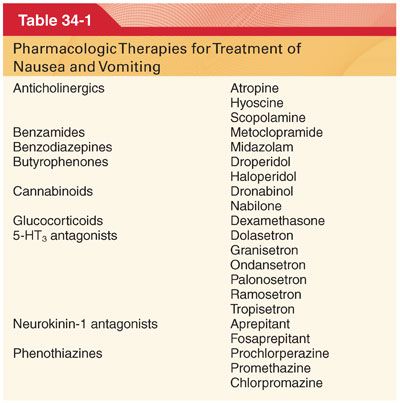
VI. Pharmacologic Interventions. A multimodal approach for prophylaxis in patients at high risk for developing PONV and as rescue therapy in patients who develop PONV in the postanesthetic care unit works well because of the complexity of systems involved in the pathogenesis of PONV (Table 34-1).
A. Anticholinergics: Scopolamine
1. Prevention of Motion-Induced Nausea and of PONV. Transdermal absorption of scopolamine provides sustained therapeutic plasma concentrations that protect against motion-induced nausea usually without introducing prohibitive side effects such as sedation, cycloplegia, or drying of secretions. Transdermal application of a scopolamine patch has been shown to exert significant antiemetic effects in patients treated with patient-controlled analgesia or epidural morphine for the management of postoperative pain.
2. Central Anticholinergic Syndrome. Scopolamine and atropine can enter the central nervous system and produce symptoms characterized as the central anticholinergic syndrome. Symptoms range from restlessness and hallucinations to somnolence and unconsciousness.
a. Physostigmine, a lipid-soluble tertiary amine anticholinesterase drug administered in doses of 15 to 60 μg/kg intravenously (IV), is a specific treatment for the central anticholinergic syndrome.
b. The central anticholinergic syndrome is often mistaken for delayed recovery from anesthesia or confusion.
3. Overdose
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


