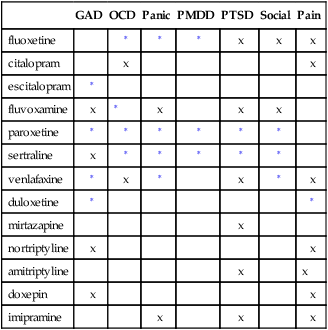
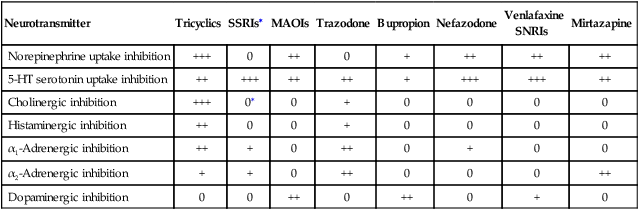
Chapter 47 Many other neurotransmitters are affected by antidepressant medications, causing numerous side effects (Table 47-2). The muscarinic system has two branches: the nicotinic and the cholinergic. Of the two, the cholinergic is by far more important. Cholinergic neurons use acetylcholine. The terms muscarinic and cholinergic often are used interchangeably. The histaminergic, α1-adrenergic, and α2-adrenergic systems also are involved in drug action. TABLE 47-2 Adverse Effects of Neurotransmitters Many mood disorders must be differentiated. See Box 47-1 for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR) diagnostic criteria for major depression. The patient with suspected major depression must have these symptoms on a daily basis for a minimum of 2 weeks. In addition, the severity of symptoms must significantly impair the patient’s quality of life and ability to perform activities of daily living (ADLs). Five types of depression or basic clusters of symptoms are known. Cognitive symptoms include memory loss, slowed thoughts, decreased attention, and inability to concentrate. Vegetative symptoms include increased or decreased sleep, altered appetite or weight, psychomotor movement, and decreased sexual function. Physical symptoms consist of fatigue, muscle tension, pain—especially head and stomach—decreased sexual drive, and weakness. Behavioral symptoms include social withdrawal, loss of interest in usual activities, crying, weeping, decreased frustration tolerance, agitation and irritability, phobias, and poor attention to self-care. Emotional symptoms occur as guilt, feelings of worthlessness, suicidal ideation or behavior, disappointment with self, hopelessness, helplessness, anxiety, and delusions or hallucinations. A complete history and physical examination are essential for the differential diagnosis of depression and for selection of the best medication for the patient. The discussion below is a brief review. Medical illnesses and medications also can contribute to the development of depression (see Tables 47-3 and 47-4). The diagnosis must rule out other factors such as drug or alcohol abuse, use of other medications, and medical conditions. Medical conditions that increase the risk of depression are cancer, chronic lung disease, heart disease, stroke, diabetes, end-stage renal disease, dementia, hypothyroidism, chronic fatigue syndrome, fibromyalgia, systemic lupus erythematosus, anxiety, and panic disorder. Also ask about past episodes of depression and hypomania and a family history of bipolar disorder. See Box 47-2 for a list of risk factors for depression. TABLE 47-3 Illnesses Commonly Occurring with Depression TABLE 47-4 Drug Classes That Produce the Side Effect of Depression All categories of antidepressant medication have a common major mechanism of action. Slight variations within a drug category may be noted. Table 47-5 shows the antidepressants as classified according to mechanism of action. These medications are discussed in terms of the order of current usage. Older medications tend to have additional side effects. Newer antidepressants demonstrate a trend toward more specifically tailored mechanisms of action. Antidepressant therapies that are not categorized as SSRIs, TCAs, or MAOIs also have been developed; these are referred to in the literature as atypical antidepressants. The drugs include bupropion (Wellbutrin), nefazodone (Serzone), and trazodone (Desyrel). TABLE 47-5 Antidepressant Classification Based on Neurotransmitter 0, No activity; +, weak activity; ++, moderate activity; +++, high activity. ∗Citalopram, fluoxetine, paroxetine, and fluvoxamine have weak cholinergic inhibition. • The American Psychiatric Association (APA) has published guidelines on the treatment of patients with major depressive disorder. These guidelines will be included as appropriate in the discussion of these drug treatment principles. They can be accessed at www.psych.orgpsychiatryonline.com. • Schulberg HC et al: Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines, Arch Gen Psychiatry 55:1121-1127, 1998. • American College of Physicians: Using second-generation antidepressants to treat depressive disorders, 2008. Available at www.annals.org/content/149/10/725.full. • Zuckerbrot RA et al: GLAD-PC Steering Group: Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management, Pediatrics 120:e1299-e1312, 2007. • Cheung AH et al: GLAD-PC Steering Group: Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management, Pediatrics 120:e1313-e1326, 2007.
Antidepressants
Class
Generic Name
Trade Name
Selective serotonin reuptake inhibitors (SSRIs)
fluoxetine ![]()
Prozac, Prozac weekly, Sarafem, generic
citalopram
Celexa, generic
escitalopram ![]()
Lexapro, generic
fluvoxamine∗
Luvox, generic
paroxetine
Paxil, generic
sertraline
Zoloft, generic
vilazodone
Viibryd
Serotonin/norepinephrine reuptake inhibitors (SNRIs)
venlafaxine hydrochloride SR ![]()
Effexor XR, generic
desvenlafaxine
Pristiq
duloxetine ![]()
Cymbalta ![]()
milnacipran
Savella
Norepinephrine/dopamine reuptake inhibitors (NDRIs)
bupropion ![]()
Wellbutrin SL, generic
Tricyclic antidepressants (TCAs)
nortriptyline ![]()
Pamelor, generic
amitriptyline
Elavil, generic
desipramine
Norpramin, generic
doxepin
Sinequan, generic
imipramine
Tofranil, generic
α2-Noradrenergic antagonists
mirtazapine ![]()
Remeron, generic
Serotonin 2 agonists/blockers/serotonin reuptake inhibitors (SARIs/SSRIs)
trazodone ![]()
Desyrel, generic
nefazodone
generic
Monoamine oxidase inhibitors (MAOIs)
phenelzine
Nardil, generic
tranylcypromine
Parnate, generic
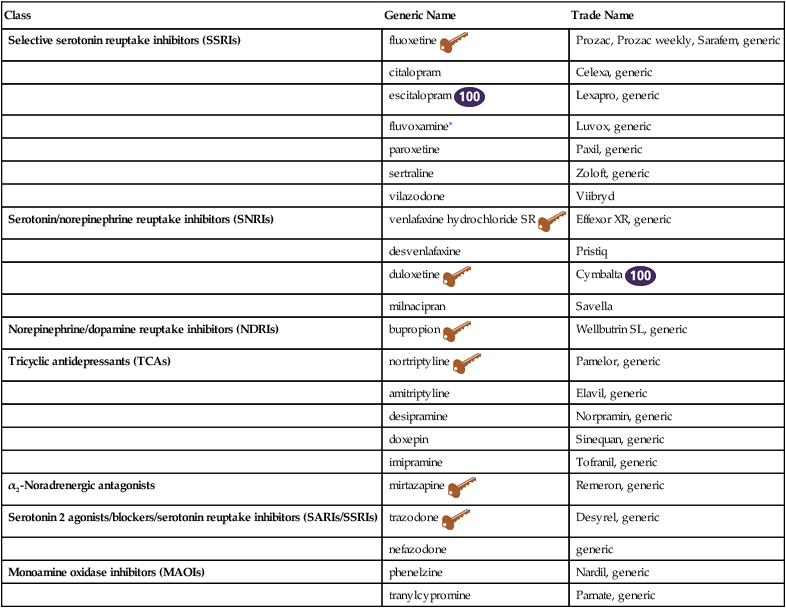
![]() Top 100 drug;
Top 100 drug; ![]() key drug. Drugs listed in order of common use.
key drug. Drugs listed in order of common use.
Therapeutic Overview
Anatomy and Physiology
Neurotransmitter
Adverse Effects
Serotonin
Anxiety, agitation, anorexia, GI distress, headache, hypotension, sexual dysfunction
Norepinephrine
Tachycardia, tremors, sexual dysfunction; augments sympathomimetics
Dopamine
Extrapyramidal symptoms, increased prolactin levels, psychosis, insomnia, anorexia, psychomotor activation
Acetylcholine
Memory dysfunction, tachycardia, blurred vision, dry mouth, urinary retention, constipation
Histamine
Sedation, hypotension, weight gain, allergy
α1-Adrenergic
Orthostatic hypotension, dizziness, cardiac conduction disturbance
α2-Adrenergic
Priapism
Disease Process
Assessment
System
Examples
Autoimmune disease
Rheumatologic disorders
CNS disease
Stroke
Dementia
Endocrine system disease
Diabetes
Thyroid disorder
Heart disease
Chronic heart failure
Myocardial infarction
Malnutrition
Vitamin deficiency
Protein/calorie deficiency
Mood disorders and psychiatric conditions
Bipolar disorders
Alcohol/drug dependency
Eating disorders
Obsessive-compulsive disorders
Anxiety disorders
Somatization disorders
Personality disorders
Psychosis
Other medical problems
Oncologic/hematologic disease
Chronic fatigue syndrome
Infectious disease
Drug Class
Specific Examples
Antihypertensives
Calcium channel blockers (diltiazem), methyldopa, nifedipine, thiazide diuretics, verapamil
Hormones
estrogen, progestins (Norplant), corticosteroids (prednisone, cortisone, ACTH), dapsone
Histamine2-receptor blockers
famotidine (Pepcid), cimetidine, metoclopramide, nizatidine
Anticonvulsants
Barbiturates, carbamazepine, clonazepam, phenytoin, valproic acid
Antiparkinsonian agents
levodopa
Cardiac medications
digitalis glycosides, HMG-CoA reductase inhibitors (statins)
Antiinfectives
Fluoroquinolone antibiotics, isoniazid, metronidazole, sulfonamides
Sedative-hypnotics
Benzodiazepines
Antineoplastics
vinblastine
NSAIDs
ibuprofen, indomethacin, naproxen, sulindac
Mechanism of Action
Neurotransmitter
Tricyclics
SSRIs∗
MAOIs
Trazodone
Bupropion
Nefazodone
Venlafaxine
SNRIs
Mirtazapine
Norepinephrine uptake inhibition
+++
0
++
0
+
++
++
++
5-HT serotonin uptake inhibition
++
+++
++
++
+
+++
+++
++
Cholinergic inhibition
+++
0∗
0
+
0
0
0
0
Histaminergic inhibition
++
0
0
+
0
0
0
0
α1-Adrenergic inhibition
++
+
0
++
0
+
0
0
α2-Adrenergic inhibition
+
+
0
++
0
0
0
++
Dopaminergic inhibition
0
0
++
0
++
0
+
0
Treatment Principles
Standardized Guidelines
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree