A. Pharmacokinetics
1. Heparin is a highly charged acidic molecule administered by intravenous (IV) or subcutaneous injection.
2. The precise pathway of heparin elimination is uncertain, and the influence of renal and hepatic disease on its pharmacokinetics is less than with other anticoagulants.
3. Heparin binds to many different proteins, which can affect its anticoagulant activity and contributes to heparin resistance.
B. Laboratory Evaluation of Coagulation. The anticoagulant response to heparin varies widely especially in critically ill patients. Different tests are used to monitor unfractionated heparin (UFH) and other anticoagulants as follows.
1. Activated Partial Thromboplastin Time
a. Heparin treatment is usually monitored to maintain the ratio of the activated partial thromboplastin time (aPTT) within a defined range of approximately 1.5 to 2.5 times normal values (typically 30 to 35 seconds).
b. An excessively prolonged aPTT (>120 seconds) is readily shortened by omitting a dose because heparin has a brief elimination half-time.
c. When low-dose heparin is used, laboratory tests may not be required to monitor treatment because the dosage and schedule are well known. However, some hospital laboratories have changed to anti-Xa assays instead of aPTT monitoring because of the variability of responses, with low-dose regimens.
2. Activated Clotting Time
a. At higher heparin concentrations like those typically used during cardiopulmonary bypass, the activated clotting time (ACT) is used to monitor anticoagulation.
b. Commercially available timing systems are used clinically to measure the ACT and are based on detecting the onset of clot formation (results between different commercial devices to measure the ACT may not be interchangeable).
c. Heparin effect and its antagonism by protamine are commonly monitored in patients undergoing cardiovascular procedures by measuring the ACT.
d. In addition to the presence of a heparin effect, the ACT may be influenced by hypothermia, thrombocytopenia, presence of contact activation inhibitors (aprotinin), and preexisting coagulation deficiencies (fibrinogen, factor XII, factor VII).
e. For cardiac surgery, a baseline value for the ACT is determined (a) before the IV administration of heparin, (b) 3 to 5 minutes after administration, and (c) at 30-minute intervals thereafter. During cardiopulmonary bypass, the target ACT value is still controversial but often considered adequate if the ACT is longer than 350 seconds, although most cardiac surgical centers target an ACT of longer than 400 seconds.
f. The need to measure ACT repeatedly is emphasized by the fourfold variation in heparin sensitivity between patients and the threefold variation in the rate at which heparin is metabolized.
III. Clinical Uses. Heparin is used extensively for multiple purposes and when administered IV has an immediate onset of action, whereas subcutaneous administration results in variable bioavailability with an onset of action in 1 to 2 hours.
A. Heparin-Induced Thrombocytopenia
1. Thrombocytopenia due to UFH is common and can begin within hours in patients exposed to heparin.
2. A more severe and even life-threatening syndrome develops in 0.5% to 6.0% of patients, manifesting as severe thrombocytopenia (50% drop in platelet count or <100,000 cells/mm3), that can be associated with thrombotic events (heparin-induced thrombocytopenia with thrombosis). This severe response typically develops after 4 to 5 days of heparin therapy and is caused by heparin-dependent antibodies to platelet factor IV that trigger platelet aggregation and result in thrombocytopenia.
B. Allergic Reactions. Heparin can cause allergic reactions, but these are rare and present in a manner typical of other hypersensitivity reactions.
C. Anticoagulation with Protamine
1. Positively charged alkaline protamine combines with the negatively charged acidic heparin to form a stable complex that is devoid of anticoagulant activity. These heparin–protamine complexes are removed by the reticuloendothelial system. Clearance of protamine by the reticuloendothelial system (within 20 minutes) is more rapid than heparin clearance and that may explain, in part, the phenomenon of heparin rebound.
2. The dose of protamine required to antagonize heparin is typically 1 mg for every 100 units of circulating heparin activity.
IV. Low-Molecular-Weight Heparins. Enoxaparin and dalteparin are two commonly administered low-molecular-weight heparins (LMWHs) derived from standard commercial-grade UFH by chemical depolymerization to yield fragments with a mean molecular weight of 4,000 to 5,000 daltons. The pharmacokinetics of enoxaparin and dalteparin between patients are more consistent than heparin because these drugs bind less avidly to proteins than heparin. This contributes to better bioavailability at low doses. Protamine does not neutralize LMWH.
A. Spinal and Epidural Hematomas. The risk of spontaneous hematoma formation may be increased in the presence of LMWH (a consideration when selecting regional anesthesia in patients being treated with LMWH preparations).
V. Prophylaxis against Venous Thromboembolism. The incidence of deep vein thrombosis is 10% to 40% among general surgery patients and higher still in high-risk surgery patient populations (orthopedic, thoracic, cardiac, vascular surgery). Thromboprophylaxis is known to effectively reduce venous thromboembolism in a cost-effective manner (subcutaneous heparin and LMWH are commonly used).
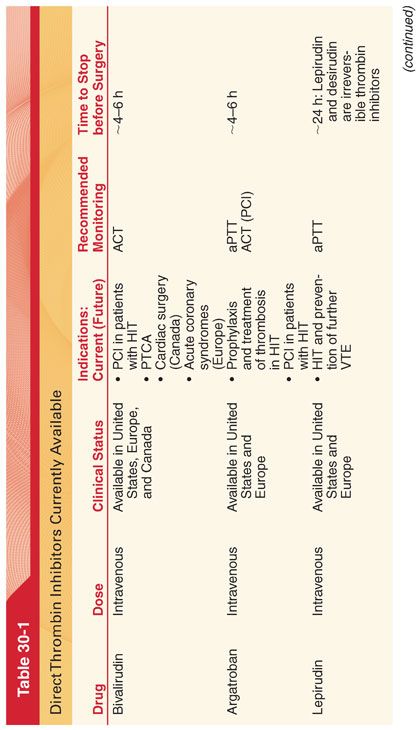
VI. Direct Thrombin Inhibitors: Parenteral Agents. An important class of anticoagulants that high-risk surgery patients at risk for HIT may receive are the direct thrombin inhibitors, including bivalirudin, argatroban, lepirudin, and desirudin (Table 30-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


