High-Yield Terms to Learn
Abnormal automaticity Pacemaker activity that originates anywhere other than in the sinoatrial node Abnormal conduction Conduction of an impulse that does not follow the path defined in Figure 14-1 or reenters tissue previously excited Atrial, ventricular fibrillation (AF, VF) Arrhythmias involving rapid reentry and chaotic movement of impulses through the tissue of the atria or ventricles. Ventricular, but not atrial, fibrillation is fatal if not terminated within a few minutes Group (class) 1, 2, 3, and 4 drugs A method for classifying antiarrhythmic drugs, sometimes called the Singh-Vaughan Williams classification; based loosely on the channel or receptor affected Reentrant arrhythmias Arrhythmias of abnormal conduction; they involve the repetitive movement of an impulse through tissue previously excited by the same impulse Effective refractory period The time that must pass after the upstroke of a conducted impulse in a part of the heart before a new action potential can be propagated in that cell or tissue Selective depression The ability of certain drugs to selectively depress areas of excitable membrane that are most susceptible, leaving other areas relatively unaffected Supraventricular tachycardia (SVT) A reentrant arrhythmia that travels through the AV node; it may also be conducted through atrial tissue as part of the reentrant circuit Ventricular tachycardia (VT) A very common arrhythmia, often associated with myocardial infarction; ventricular tachycardia may involve abnormal automaticity or abnormal conduction, usually impairs cardiac output, and may deteriorate into ventricular fibrillation; for these reasons it requires prompt management
Pathophysiology
What Is an Arrhythmia?
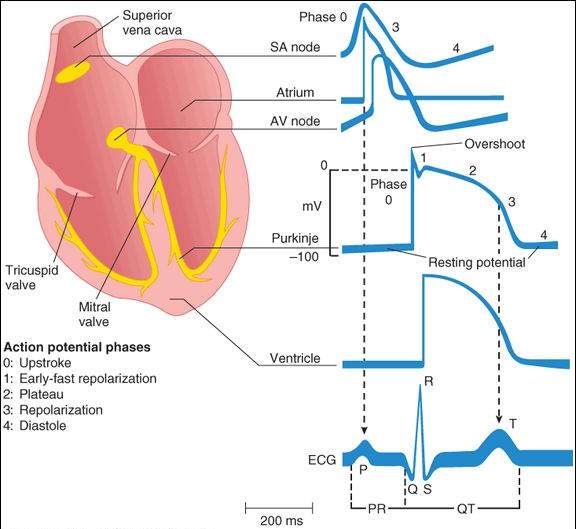
Normal electrical cardiac function (normal sinus rhythm, NSR) is dependent on generation of an impulse in the normal sinoatrial (SA) node pacemaker and its conduction through the atrial muscle, through the atrioventricular (AV) node, through the Purkinje conduction system, to the ventricular muscle (Figure 14-1). Normal pacemaking and conduction require normal action potentials (dependent on sodium, calcium, and potassium channel activity) under appropriate autonomic control. Arrhythmias (also called dysrhythmias) are therefore defined by exclusion, that is, any rhythm that is not normal sinus rhythm is an arrhythmia.
FIGURE 14-1
Schematic representation of the heart and normal cardiac electrical activity (intracellular recordings from areas indicated and ECG). The ECG is the body surface manifestation of the depolarization and repolarization waves of the heart. The P wave is generated by atrial depolarization, the QRS by ventricular muscle depolarization, and the T wave by ventricular repolarization. The PR interval is a measure of conduction time from atrium to ventricle through the atrioventricular (AV) node, and the QRS duration indicates the time required for all of the ventricular cells to be activated (ie, the intraventricular conduction time). The QT interval reflects the duration of the ventricular action potential. SA, sinoatrial.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 14-1.)
Arrhythmogenic Mechanisms
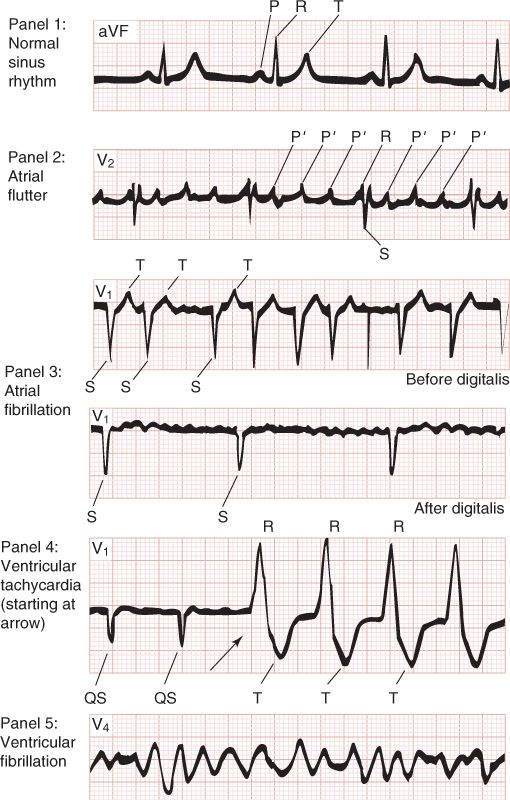
Abnormal automaticity and abnormal (reentrant) conduction are the 2 major mechanisms for arrhythmias. A few of the clinically important arrhythmias are atrial flutter, atrial fibrillation (AF), atrioventricular nodal reentry (a common type of supraventricular tachycardia [SVT]), premature ventricular beats (PVBs), ventricular tachycardia (VT), and ventricular fibrillation (VF). Examples of electrocardiographic (ECG) recordings of normal sinus rhythm and some of these common arrhythmias are shown in Figure 14-2. Torsade de pointes is a ventricular arrhythmia of great pharmacologic importance because it is often induced by antiarrhythmic and other drugs that change the shape of the action potential and prolong the QT interval. It has the ECG morphology of a polymorphic ventricular tachycardia, often displaying waxing and waning QRS amplitude. Torsade is also associated with long QT syndrome, a heritable abnormal prolongation of the QT interval caused by mutations in the IK or INa channel proteins.
FIGURE 14-2
Typical ECGs of normal sinus rhythm and some common arrhythmias. Major waves (P, Q, R, S, and T) are labeled in each electrocardiographic record except in panel 5, in which electrical activity is completely disorganized and none of these deflections are recognizable.
(Modified and reproduced, with permission, from Goldman MJ: Principles of Clinical Electrocardiography, 11th ed. McGraw-Hill, 1982.)
Normal Electrical Activity in the Cardiac Cell
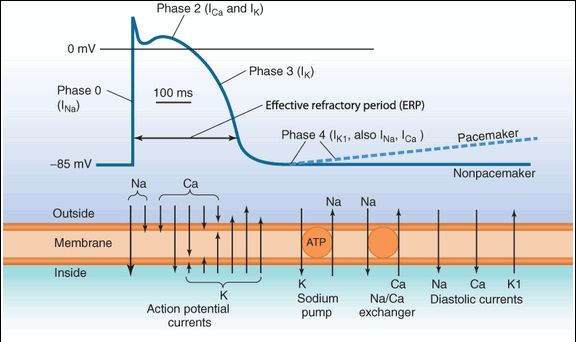
The cellular action potentials shown in Figure 14-1 are the result of ion fluxes through voltage-gated channels and carrier mechanisms. These processes are diagrammed in Figure 14-3. In most parts of the heart, sodium current (INa) dominates the upstroke (phase 0) of the action potential (AP) and is the most important determinant of its conduction velocity. After a very brief activation, the sodium current enters a more prolonged period of inactivation. In the calcium-dependent AV node, calcium current (ICa) dominates the upstroke and the AP conduction velocity. The plateau of the AP (phase 2) is dominated by calcium current (ICa) and one or more potassium-repolarizing currents (referred to as a class as IK). At the end of the plateau, IK causes rapid repolarization (phase 3).
FIGURE 14-3
Components of the membrane action potential (AP) in a typical Purkinje or ventricular cardiac cell. The deflections of the AP, designated as phases 0-3, are generated by several ionic currents. The actions of the sodium pump and sodium-calcium exchanger are mainly involved in maintaining ionic steady state during repetitive activity. Note that small but significant currents occur during diastole (phase 4) in addition to the pump and exchanger activity. In non-pacemaker cells, the outward potassium current during phase 4 is sufficient to maintain a stable negative resting potential as shown by the solid line at the right end of the tracing. In pacemaker cells, however, the potassium current is smaller and the depolarizing currents (sodium, calcium, or both) during phase 4 are large enough to gradually depolarize the cell during diastole (dashed line). ATP, adenosine triphosphate.
The refractory period of most cardiac cells (the sodium-dependent cells) is a function of how rapidly sodium channels recover from inactivation. Recovery from inactivation depends on both the membrane potential, which varies with repolarization time and the extracellular potassium concentration, and on the actions of drugs that bind to the sodium channel (ie, sodium channel blockers). The carrier processes (sodium pump and sodium-calcium exchanger) contribute little to the shape of the AP (but they are critical for the maintenance of the ion gradients on which the sodium, calcium, and potassium currents depend). Antiarrhythmic drugs act on 1 or more of the 3 major currents (INa, ICa, IK) or on the  adrenoceptors that modulate these currents. Similarly, in the calcium-dependent AV node, the duration of refractoriness is dependent on the rate of recovery from inactivation of the calcium channels.
adrenoceptors that modulate these currents. Similarly, in the calcium-dependent AV node, the duration of refractoriness is dependent on the rate of recovery from inactivation of the calcium channels.
Drug Classification
The antiarrhythmic agents are usually classified using a system loosely based on the channel or receptor involved. As indicated by the figure on the first page of this chapter, this system specifies 4 groups or classes, usually denoted by the numerals 1 through 4, plus a miscellaneous group (Table 14-1 and Drug Summary Table).
1. Sodium channel blockers
2. Beta-adrenoceptor blockers
3. Potassium channel blockers
4. Calcium channel blockers
TABLE 14-1 Properties of the prototype antiarrhythmic drugs.
Drug Group PR Interval QRS Duration QT Interval Procainamide, disopyramide, quinidine 1A  or
or  a
a



 Lidocaine, mexiletine 1B — —b
Lidocaine, mexiletine 1B — —b
— Flecainide 1C  (slight)
(slight) 
 — Propranolol, esmolol 2
— Propranolol, esmolol 2 
 — — Amiodarone 3, 1A, 2, 4
— — Amiodarone 3, 1A, 2, 4 





 Ibutilide, dofetilide 3 — —
Ibutilide, dofetilide 3 — — 

 Sotalol 3, 2
Sotalol 3, 2 
 —
— 

 Verapamil 4
Verapamil 4 
 — — Adenosine Misc
— — Adenosine Misc 

 — —
— —
aPR interval may decrease owing to antimuscarinic action or increase owing to channel-blocking action.
bLidocaine, mexiletine, and some other group 1B drugs slow conduction through ischemic, depolarized ventricular cells but not in normal tissue.
The miscellaneous group includes adenosine, potassium ion, and magnesium ion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree