Angiomyomatous Hamartoma
Carlos E. Bueso-Ramos, MD, PhD
Key Facts
Terminology
Benign smooth muscle proliferation that begins in hilum and extends into medulla and cortex of lymph node
Involves inguinal lymph nodes almost exclusively
Clinical Issues
Wide age range; male predominance
Lymph node enlargement is often of long duration
Pain, edema, or swelling of ipsilateral limb may be present
Lesion clinically innocuous
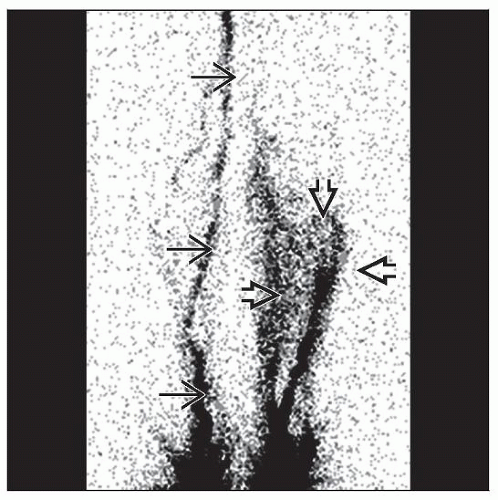
Image Findings
Poorly circumscribed mass with heterogeneous echo levels
Extensive lymph node abnormalities by lymphoscintigraphy studies
Microscopic Pathology
Characterized by extensive lymph node parenchymal replacement by
Smooth muscle with absence of cellular fascicles
Blood vessels
Fibrous tissue
No mitoses
Ancillary Tests
Immunohistochemistry
Smooth muscle cells: H-caldesmon(+), muscle specific actin(+), desmin(+), CD34(-)
Endothelial cells: CD31(+), CD34(+)
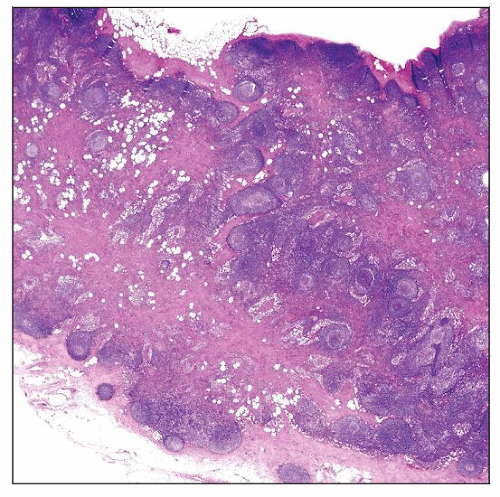 Hematoxylin and eosin stain shows angiomyomatous hamartoma extensively replacing the lymph node parenchyma. |
TERMINOLOGY
Abbreviations
Angiomyomatous hamartoma (AH)
Definitions
Benign smooth muscle proliferation that begins in hilum and extends into medulla and cortex of lymph node
Involves inguinal lymph nodes almost exclusively
ETIOLOGY/PATHOGENESIS
Unknown
Unknown but may represent
Acquired hamartomatous lesion
Unusual reparative reaction to previous lymph node inflammation
Result of interference with normal lymphatic drainage
CLINICAL ISSUES
Epidemiology
Age
Mean: 42 years
Range: 3-80 years
Gender
M:F ratio = 5:1
Site
Edema or swelling of ipsilateral limb sometimes accompanies lymphadenopathy
Lesion is clinically innocuous but may recur after excision
Presentation
Patients present with enlarged inguinal lymph nodes
Lymph nodes can be matted
Lymphadenopathy is often of long duration
Pain and swelling
Occurrence
13 of 17 cases developed in inguinal lymph nodes
2 cases in femoral lymph nodes
1 case each in popliteal and cervical lymph nodes, respectively
Treatment
Surgical approaches