Angiomatoid Fibrous Histiocytoma
Khin Thway, BSc, MBBS, FRCPath
Key Facts
Terminology
Rare neoplasm of intermediate biologic potential
Most often arises in extremities of children and young adults
Histologically often confused with both benign and malignant lesions
3 characteristic translocations
Clinical Issues
Slowly growing
Mostly indolent
15% recur, 1% metastasize
Microscopic Pathology
Fibrous and lymphoplasmacytic cuff
Dense peripheral lymphoplasmacytic cuff in up to 80%
Histiocyte-like and spindle cells
In sheets, short fascicles, occasional storiform distributions
Cells with bland, vesicular, ovoid to spindled nuclei
Blood-filled spaces
Some show marked pleomorphism and mitotic activity
Ancillary Tests
Desmin positivity in 1/2 of cases
Specific translocations
Top Differential Diagnoses
Aneurysmal benign fibrous histiocytoma
Spindle cell hemangioma
Kaposi sarcoma
Pleomorphic sarcoma (MFH)
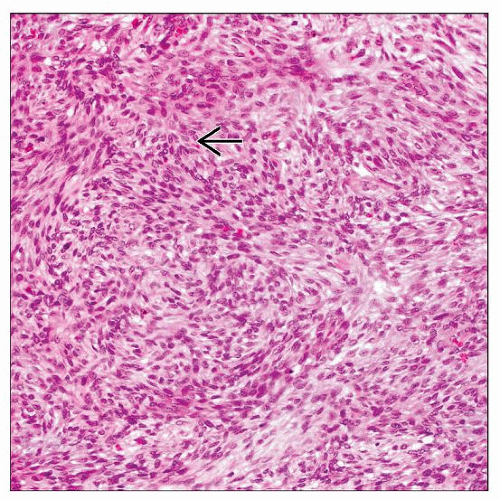
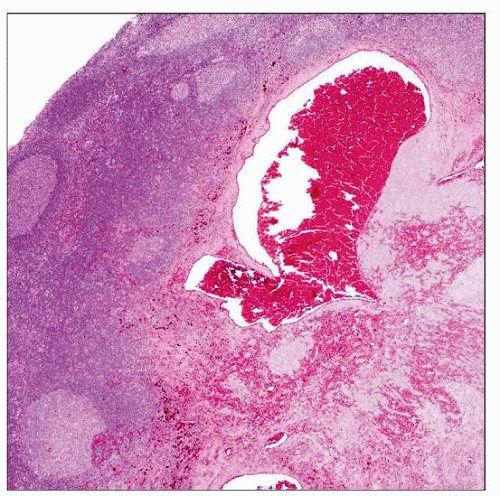 Angiomatoid fibrous histiocytoma is a circumscribed lesion with a pronounced lymphoid cuff, including prominent germinal centers. This appearance may mimic that of a tumor metastatic to a lymph node. |
TERMINOLOGY
Abbreviations
Angiomatoid fibrous histiocytoma (AFH)
Synonyms
Originally termed “angiomatoid malignant fibrous histiocytoma”
Term “malignant” removed due to indolent behavior
Unrelated to malignant fibrous histiocytoma (MFH)/pleomorphic sarcoma group of neoplasms
Definitions
Rare neoplasm of intermediate biologic potential with 3 characteristic translocations
ETIOLOGY/PATHOGENESIS
Lineage Unknown
Desmin expression
Suggests myoid or myofibroblastic differentiation
Endothelial or histiocytic differentiation unlikely
Postulated nodal fibroblastic reticulum cell differentiation
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Accounts for approximately 0.3% of all soft tissue neoplasms
Age
Infancy to 8th decade
Predominantly in children and young adults
Gender
Slight female predilection
Site
Extremities
Trunk
Head and neck
1 primary intracerebral case reported
Very rarely other sites
Lung, mediastinum, retroperitoneum, ovary, vulva
Usually superficial
Deep dermis and subcutis
Few arise deeply
Presentation
Slowly growing, painless mass
Usually small
Most often 2-4 cm
Constitutional symptoms in subset
Malaise
Pyrexia
Anemia
Due to possible tumoral cytokine production
Treatment
Surgical approaches
Wide excision
Usually curative
Radiotherapy and chemotherapy
For rare metastatic or unresectable tumors
Prognosis
Excellent in most cases
Majority of lesions indolent
Regional recurrence rate up to 15%
Metastasis rate of approximately 1%
No firm morphologic or clinical indicators of behavior
Infiltrative margin and deep location can predict recurrence
MACROSCOPIC FEATURES
General Features
Firm
Circumscribed
Blood-filled cystic cavities
Sections to Be Submitted
Lesion should be thoroughly sampled
Small lesions should be submitted in entirety
MICROSCOPIC PATHOLOGY
Histologic Features
Circumscribed, lobulated mass
Fibrous pseudocapsule
Dense peripheral lymphoplasmacytic cuff
Present in up to 80%
Mixture of B- and T cells
Germinal center formation may be present
Cells with bland, vesicular, ovoid to spindled nuclei
Sheets
Short fascicles
Occasional storiform patterns
Ovoid or spindle forms may predominate
Mitoses infrequent
Hemorrhagic cavities
Lack endothelial lining
Some show marked pleomorphism and mitotic activity
Not shown to be associated with outcome
Giant cells in some cases
Clear cells and reticular and pulmonary edema-like patterns are rarely described
Predominant Pattern/Injury Type
Circumscribed
Cystic, macroscopic
Predominant Cell/Compartment Type
Mesenchymal
ANCILLARY TESTS
Cytogenetics
3 characteristic translocations identified
(2;22)(q33;q12) EWSR1-CREB1
Most common gene fusion
(12;16)(q13;p11) FUS-ATF1
(12;22)(q13;q12) EWSR1-ATF1
Fusion type not thought to be related to tumor site
No correlation between type of fusion gene and clinicopathologic features
All these translocations also seen in clear cell sarcomas
Clear cell sarcoma (of tendons and aponeuroses)
Clear cell sarcoma-like tumor of the gastrointestinal tract
Morphologically and clinically distinct neoplasms
In Situ Hybridization
Translocated chromosomes can be identified by FISH
PCR
Fusion gene transcripts can be identified by RT-PCR
Frozen or paraffin-embedded material
Electron Microscopy
No diagnostic ultrastructural findings
DIFFERENTIAL DIAGNOSIS
Aneurysmal Dermatofibroma (Benign Fibrous Histiocytoma)
Usually intradermal
Epidermal hyperplasia overlying lesion
Tumor is not well-circumscribed
Peripheral collagen bundles
Mixed cell population
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree