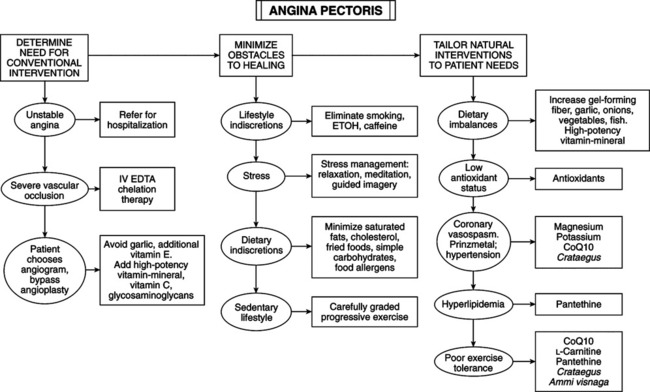
• Squeezing pain or pressure in the chest appearing immediately after exertion. Other precipitating factors include emotional tension, cold weather, or a large meal. Pain may radiate to the left shoulder blade, left arm, or jaw. The pain typically lasts for only 1-20 minutes. • Stress, anxiety, and high blood pressure typically are present. • The majority demonstrate an abnormal electrocardiographic reading (transient ST-segment depression) in response to light exercise (stress test). • Prinzmetal’s variant angina: most common form of coronary artery spasm, not caused by plaque, occurs at rest or at odd times during day or night; more common in women younger than 50. • Magnesium insufficiency–induced coronary artery spasm: more common in men than in women; important cause of MI and significant in angina pectoris. • Angiograms: landmark study of patients told they needed angiograms to determine degree of blockage and need for bypass surgery or angioplasty. Noninvasive tests (exercise stress test, echocardiogram, 24-hour Holter monitor) revealed that 80% did not need catheterization. These patients had an annual fatal MI rate over a 5-year period much lower than mortality rates for surgical procedures. Noninvasive testing to determine the functional state of the heart is far more important in determining indicated therapy than is dangerous search for blocked arteries. If heart is dysfunctional, then angiogram is indicated to ascertain need for surgery. Blockages found by angiogram are usually not relevant to risk of MI. • Coronary Artery Surgery Study (CASS): patients with heart disease who had healthy hearts, but one, two, or all three major heart vessels blocked, did surprisingly well without surgery. Regardless of number or severity of blockages, each group had the same low annual death rate of 1%. Severity of blockage does not estimate reduction in blood flow; no correlation between blood flow and severity of blockage; angiogram did not provide clinically relevant information. Critical factor: how well left ventricle is working, not degree of blockage or number of arteries affected. Bypass only helpful when ejection fraction is <40%. (Greater than 50% is adequate for circulatory needs.) Studies: 61% of patients who underwent bypass surgery had nervous system disorders as a result; 2%-5% die during or soon after operation; 10% have MIs. • Dietary and lifestyle changes: significantly reduce risk of MI and other causes of death from atherosclerosis (Textbook, “Atherosclerosis”). Nutritional supplements and botanical medicines improve heart function in even the most severe angina cases. IV EDTA chelation: controversial, but clinical research has proven its efficacy. • When cardiac procedure is unavoidable, goal is to prevent damaging effects and restenosis: high-potency multiple vitamin-mineral, additional vitamin C (500 mg t.i.d.+) and CoQ10 (100 mg q.d. 2 weeks before surgery and for 3 months after); garlic and high dosages vitamin E (>200 IU) to be avoided before surgery because of inhibition of platelet aggregation. Vitamin C plummets by 70% 24 hours after bypass surgery and persists for 2 weeks. After surgery, vitamin E and carotene levels do not change significantly—fat-soluble and retained longer; vitamin C depletion may deteriorate wound repair and defenses against free radicals and infection; CoQ10 can prevent oxidative damage during reperfusion. (Return of blood after bypass surgery induces oxidative damage to vascular endothelium and myocardium, increasing risk for subsequent coronary artery disease.) CoQ10 (150 mg q.d. for 7 days before surgery) prevents reperfusion injury and lowers incidence of ventricular arrhythmias during recovery period. Mixture of purified bovine aortic glycosaminoglycans (dermatan sulfate, heparin sulfate, hyaluronic acid, chondroitin sulfate) (100 mg q.d.) helps prevent reperfusion injury and restore structural integrity of endothelium.
Angina Pectoris
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
THERAPEUTIC CONSIDERATIONS
Coronary Angiogram, Artery Bypass Surgery, and Angioplasty
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Angina Pectoris