13 Angina pectoris
Salient features
History
• Have you ever had any pain or discomfort in the chest?
• How would you describe the chest discomfort (heavy, burning, tightness, stabbing, pressure)?
• Do you get this on walking at ordinary pace on the level or does it come when you walk uphill or hurry?
• When you get the pain/discomfort, do you stop, slow down or continue at the same pace?
• Does the pain/discomfort go away when you stand still? (It is typically relieved by rest or glyceryl trinitrate within 10 min.)
• Where do you get this pain? (Because angina is a visceral sensation, it is poorly localized and, therefore, patients rarely point to the location of their discomfort with one finger.)
• Does it radiate elsewhere (e.g. arms, jaw, epigastrium)?
• Does food or cold weather bring on the pain?
• Ask about risk factors such as smoking, diabetes, hypertension, family history of ischaemic heart disease.
• Ask about past medical history of coronary artery disease.
Questions
How is angina graded by the Canadian Cardiovascular Society?
There are four functional classes:
• I: angina occurs only with strenuous or rapid or prolonged exertion
• II: slight limitation of ordinary activity (e.g. climbing more than one flight of ordinary stairs at a normal pace and in normal conditions)
• III: marked limitation of ordinary activity (e.g. climbing more than one flight in normal conditions)
• IV: inability to carry out any physical activity without discomfort—anginal syndrome may be present at rest.
How would you investigate a patient with angina pectoris?
• Haemoglobin: anaemia aggravates angina
• Rest ECG to detect left ventricular hypertrophy, prior Q-wave MI or ST-T changes
• Rest echocardiogram is carried out only when there is clinical suspicion of aortic stenosis or hypertrophic cardiomyopathy
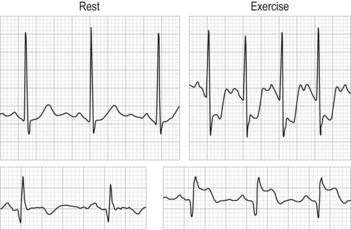
• Exercise ECG can precipitate symptoms, document workload at onset and record any associated ECG abnormality (≥1 mm of horizontal or downsloping ST-segment depression or elevation for ≥60 to 80 ms after the end of the QRS complex) or arrhythmia (Fig. 13.1)
• Exercise myocardial perfusion imaging or exercise echocardiography is used in patients where considerations of functional significance of lesions or myocardial viability are important or who have one of the following baseline ECG abnormalities:
• Coronary angiography: provides detailed anatomical information about site and severity of luminal narrowing caused by coronary atherosclerosis and less-common non-atherosclerotic causes such as coronary artery spasm, coronary anomaly, primary coronary artery dissection and radiation-induced coronary vasculopathy.
How would you treat a patient with chronic stable angina pectoris?
Treatment is remembered with the mnemonic ABCDE (Circulation 1999;99:2829–48).
A: aspirin, antianginal therapy and ACE inhibitor therapy. Aspirin has been shown to reduce the incidence of non-fatal MI and the overall incidence of cardiac events, although overall death rate and the incidence of fatal MI were similar to those obtained with placebo in the Swedish Angina Pectoris Aspirin Trial (SAPAT) study. Ramipril up to 10 mg once a day should be offered to all patients in view of the new HOPE trial. Antianginal therapy includes nitrates, ranalozine and nicorandril.
B: beta-blocker and blood pressure
C: cigarette smoking and cholesterol (clopidogrel)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree