Anatomy of the Head and Neck
Aaron Ruhalter
Surface anatomy is the relationship between structures that are visible and/or palpable with structures that are not visible and/or palpable. Visible and/or palpable structures in the neck include the following:
Sternocleidomastoid (sternomastoid) muscle that attaches to the superior aspect of the manubrium sternum by a tendinous head and from the medial third of the clavicle by a muscular head. It passes superiorly in a lateral, and then posterior, direction. Its superior attachment is to the mastoid process, and the lateral end of the superior nuchal line. Unilateral contraction of the muscle approximates the ear to the ipsilateral shoulder, while rotating the chin to the contralateral side. Bilateral contraction of the muscle can result in either flexion or extension of the head. If the head is slightly flexed, bilateral contraction will result in increased flexion. If the head is slightly extended, bilateral contraction will result in increased extension. The pulsation of the carotid artery is palpable, anterior to the edge of the muscle.
Trapezius muscle that has a very broad origin from the medial portion of the superior nuchal line, external occipital protuberance, ligamentum nuchae, spinous processes, and the supraspinous ligaments of the thoracic vertebrae. The muscle fibers converge and insert on the lateral third of the clavicle and the acromion process of the scapula. Because of the extensive origin of the muscle, differential contraction will create different movements. Contraction of the upper fibers will cause elevation of the scapula. Depression of the scapula is created by contraction of the inferior fibers. The middle fibers will cause the medial edge of the scapula to approach the midline. The external branch of the accessory nerve provides innervation to the trapezius and sternocleidomastoid muscles. Branches from the second and third cervical nerves provide added innervation.
Mastoid process.
Ramus of mandible.
Hyoid bone, palpable in the midline of the neck when the mandible is slightly depressed. It is located at the level of the third cervical vertebra. The greater horn of the hyoid bone can be traced to its lateral termination. This is the approximate level of origin of the lingual branch of the external carotid artery. The superior thyroid branch arises just inferior to this point, and the facial branch begins just superior to the same palpable landmark.
Fused laminae of the thyroid cartilage. The upper edge of this palpable structure is situated at the level of the fourth cervical vertebra. It represents the site of bifurcation of the common carotid artery.
Arch of the cricoid cartilage, palpable below the inferior end of the thyroid laminae. A small defect separates them. The cricoid cartilage represents an “anatomical bonanza” because it is a landmark for many anatomical occurrences. It may be referred to as the “cricoid plane.”
The larynx ends, and the trachea begins.
The pharynx ends, and the esophagus begins.
The cricoid cartilage is at the level of the sixth cervical vertebra.
The intermediate tendon of the omohyoid muscle is found anterior to the carotid sheath.
The inferior thyroid artery passes posterior to the carotid sheath on its way to the lateral lobe of the thyroid gland.
The middle cervical sympathetic ganglion lies on the transverse mass of the sixth cervical vertebra.
The recurrent laryngeal nerve enters the larynx.
The ansa cervicalis is found anterior to the carotid sheath.
The vertebral artery enters a foramen in the transverse mass of the sixth cervical vertebra. This occurs at the apex of a muscular triangle formed by the anterior scalene and longus coli muscles. The base of the triangle is the first portion of the subclavian artery.
TThe superior pair of parathyroid glands is often found at this level.
Upper tracheal rings that are palpable between the cricoid cartilage and the superior edge of the manubrium sternum.
Superior edge of the manubrium of the sternum. It is at the level of the second thoracic vertebra.
Structure of the Neck
Skeletal Background
The cervical portion of the vertebral column creates the skeletal background. It is composed of seven cervical vertebrae, with a characteristic anterior convex curvature. Vertebrae C3 through C6 are considered to be typical cervical vertebrae. Vertebrae C1, C2, and C7 are atypical cervical vertebrae. C1 (atlas) has no body. C2 (axis) has incorporated the body of C1 in its structure. The combination of the two bodies results in a tooth-like projection called the odontoid process, or dens epistrophe.
This provides an axis of rotation for the skull on the atlas. C7 has a large transverse mass with a primitive foramen and a prominent spinous process (vertebra prominens). The typical cervical vertebrae have a bifid spinous process and a distinct foramen in the transverse mass. There are anterior and posterior tubercles related to the transverse mass. The first rib must be included in the skeletal background. Many of the neck structures are attached to, or pass over, the first rib. The superior surface of the first rib is flattened. This will avoid trauma to the neurovascular structures that travel over it. Midway between the vertebral and the sternal ends of this rib is the scalene tubercle, point of insertion of the anterior scalene muscle. A vascular sulcus is found on both sides of the scalene tubercle. The anterior sulcus provides passage for the subclavian vein. The subclavian artery passes over the posterior sulcus. The anterior scalene muscle attaches to the first rib between the subclavian vessels. The middle scalene muscle attaches to the first rib posterior to the groove for the subclavian artery. Therefore, the subclavian artery passes through the scalene triangle that is created by the anterior and middle scalene muscles. This area is referred to as the root of the neck. It will be described in more detail later in this chapter.
Ligamentous Background
The ligamentous background includes supporting structures for the atlanto-occipital and atlantoaxial joints. The anterior longitudinal ligament is found on the anterior aspect of the vertebral bodies. It extends
from the atlas down to the upper sacral segment. It is attached to the intervertebral disc and that portion of the vertebral body lying just superior and inferior to the disc. The nuchal ligament covers the spinous processes of all the cervical vertebrae.
from the atlas down to the upper sacral segment. It is attached to the intervertebral disc and that portion of the vertebral body lying just superior and inferior to the disc. The nuchal ligament covers the spinous processes of all the cervical vertebrae.
Muscular Background
The muscular background includes muscles that are attached to the anterior aspect of the vertebra (anterior vertebral) and muscles that are attached to the lateral mass of the vertebra (lateral vertebral). Both of these groups are combined and are referred to as prevertebral muscles. The longus coli and longus capitis muscles are anterior to the vertebral column. The longus coli is a complex muscle that is attached inferiorly to the upper thoracic portion of the anterior longitudinal ligament. These lower fibers pass superolaterally and attach to the transverse masses of the typical cervical vertebrae. Fibers of this same muscle then pass superomedially and attach to the anterior portion of the arch of the atlas. There are vertical fibers of this same muscle that lie between the two oblique portions laterally and the anterior longitudinal ligament medially.
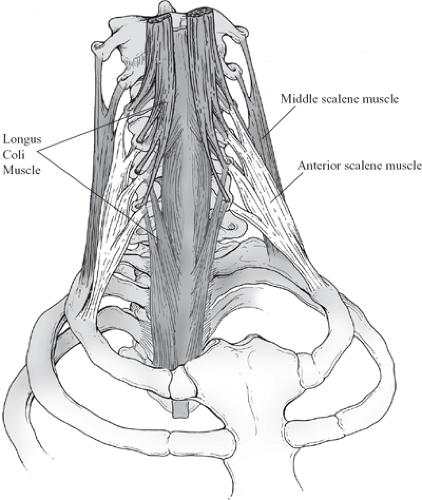
The longus capitis muscle lies anterior to the superomedial fibers of the longus coli muscle. It passes from the base of the skull to the tubercles of the typical cervical vertebrae. The muscles that are lateral vertebral in position are the levator scapula, middle, and anterior scalene muscles. The levator scapula muscle is the most posterior of this lateral group. It arises from the posterior tubercles of the transverse masses of the first four cervical vertebrae, descends, and attaches to the superior portion of the vertebral border of the scapula. The middle scalene muscle is on a more anterior plane (Fig. 1).
The middle scalene muscle may be attached to the posterior tubercles of all cervical vertebrae. It descends and affixes to the superior flattened surface of the first rib, posterior to the groove for the subclavian artery. A few muscle fibers extend down to the second rib and create the posterior scalene muscle. The most anterior of the lateral vertebral muscles is the anterior scalene (Fig. 1). It arises from the anterior tubercles of the transverse masses of the typical cervical vertebrae and attaches below to the scalene tubercle of the first rib. It is in the same frontal plane as the longus capitis muscle. The anterior vertebral muscles will flex the cervical spine. The lateral vertebral muscles will cause lateral bending of the same area. Motor innervation is provided by ventral rami of cervical nerves.
Nerve Background
The nerve layer should now be inserted. The nerves and the muscles are intimately related, so that the term “neuromuscular layer” is appropriate. The cervical and brachial plexuses and the cervical sympathetic chains are now encountered as we continue the reconstruction of the neck.
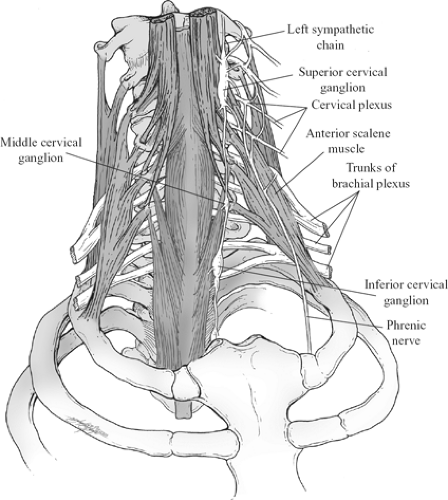
The cervical sympathetic chain consists of three ganglia with connecting branches. The superior ganglion is the largest, and it is found on the transverse mass of the second and third cervical vertebrae. It is >1 in. long and lies on the longus capitis muscle, posterior to the carotid sheath. The middle cervical ganglion is the smallest and lies on the transverse mass of the sixth cervical vertebra. The inferior cervical ganglion is related to the vertebral end of the first rib and the transverse mass of the seventh cervical vertebra. It frequently joins with the first thoracic ganglion to form a dumbbell-shaped structure called the cervicothoracic, or stellate, ganglion. Stellate refers to the star-like appearance created by the multiple branches that are emitted. It is posterior to the vertebral artery. At times, branches from the middle cervical ganglion will form a loop around the subclavian artery before entering the inferior ganglion. This is referred to as the ansa subclavia.
The cervical plexus is formed by the ventral rami of the first four cervical nerves. These nerves connect to each other by forming loops that lie in the interval between the levator scapula, or the middle scalene, muscle posteriorly, and the longus capitis or its inferior continuation, the anterior scalene muscle, anteriorly (Fig. 2).
Each of the first four cervical ventral rami receives a branch from the superior cervical ganglion. The cervical nerves lie within the prevertebral fascia. The cervical plexus provides muscular and cutaneous innervation. There are cutaneous branches from a superficial cervical plexus and muscular branches from a deep cervical plexus. The cutaneous branches will be described with the posterior triangle. Muscular branches innervate the prevertebral muscles. In addition, a branch from C1 travels with the hypoglossal nerve and gives rise to the superior limb (descending hypoglossal nerve) of the ansa cervicalis. Branches from C2 and C3 will form the inferior limb (descending cervical nerve). The two limbs unite and form the ansa cervicalis. This nerve loop is on the anterior aspect of the carotid sheath, in the cricoid plane. Branches arise from the ansa cervicalis that provide motor innervation to the strap muscles in the muscular triangle. Other branches of C1,
traveling with the hypoglossal nerve, provide motor innervation to the thyrohyoid and geniohyoid muscles. A branch from C4 descends on the anterior surface of the anterior scalene muscle, within the prevertebral fascia. It is the phrenic nerve and it may receive branches from C3 and C5. It is, at first, seen on the lateral aspect of the anterior scalene muscle, but as it descends it passes obliquely across the anterior surface of the muscle and reaches its medial edge in the root of the neck. It then passes anterior to the subclavian artery and courses medial to the internal mammary artery before entering the thorax. It provides sensory and motor innervation to the respiratory diaphragm (Fig. 2). There are some proprioceptive branches arising from the cervical plexus that pass to the sternocleidomastoid and trapezius muscles.
traveling with the hypoglossal nerve, provide motor innervation to the thyrohyoid and geniohyoid muscles. A branch from C4 descends on the anterior surface of the anterior scalene muscle, within the prevertebral fascia. It is the phrenic nerve and it may receive branches from C3 and C5. It is, at first, seen on the lateral aspect of the anterior scalene muscle, but as it descends it passes obliquely across the anterior surface of the muscle and reaches its medial edge in the root of the neck. It then passes anterior to the subclavian artery and courses medial to the internal mammary artery before entering the thorax. It provides sensory and motor innervation to the respiratory diaphragm (Fig. 2). There are some proprioceptive branches arising from the cervical plexus that pass to the sternocleidomastoid and trapezius muscles.
As we pass inferiorly in the cervical region, the nerves now encountered will consist of the roots and trunks of the brachial plexus. The brachial plexus is created by the ventral rami of C5 through T1. These roots will form three trunks. C5 and C6 join to form the upper trunk. The C7 root will become the middle trunk, and roots C8 and T1 will merge and form the lower trunk. These roots and trunks pass between the middle and the anterior scalene muscles. The lower trunk is draped over the first rib immediately posterior to the subclavian artery (Fig. 2).
The subclavian vein, unlike the accompanying artery, does not pass between the scalene muscles. It passes anterior to the anterior scalene muscle. Enclosing the skeletal background and the neuromuscular layer is the prevertebral portion of the deep cervical fascia. The neurovascular structures will pierce the deep cervical fascia and drag a portion of it along with them, creating the axillary, or cervicoaxillary, sheath.
Fascia of the Neck
The cervical fascia is composed of superficial and deep layers. The superficial fascia is not well developed and not easy to find. It consists of fat and some connective tissue. The platysma muscle is in the superficial fascia. It arises inferiorly from the fascia of the pectoralis major muscle and its fibers converge as they ascend to their insertion in the inferior part of the mandibular region. Some of the muscle fibers ascend and mix with the intrinsic depressor muscles of the lips. The cutaneous nerves and the superficial veins course below this muscle of facial expression. The cervical branch of the facial nerve innervates this muscle.
The deep cervical fascia consists of several layers. The superficial, or investing, layer of the deep cervical fascia splits to invest the trapezius and sternocleidomastoid muscles and the submandibular and parotid glands. It creates a complete tube that surrounds the neck. The deep layer of the deep cervical fascia, or prevertebral fascia, encloses the vertebral column and the attached erector spinae and prevertebral muscles and proximal portions of the cervical and brachial plexuses. It creates a complete tube.
The pretracheal fascia creates a tube that encircles the pharynx and esophagus, larynx and trachea, and the thyroid and parathyroid glands. The buccopharyngeal fascia is the posterior extension of the pretracheal fascia that covers the constrictor muscles of the pharynx. It is in contact with the anterior, or prevertebral, portion of the prevertebral fascia. This potential space between the prevertebral and the buccopharyngeal fascia layers extends from the neck down to the mediastinum. This retropharyngeal space can serve as a pathway for the spread of an infection from the neck to the thorax. The middle cervical fascia extends from the hyoid bone to the sternum. It encompasses all the strap muscles. This fascia layer extends laterally to the omohyoid muscle and therefore is only related to the muscular and subclavian triangles.
The carotid sheath is a protective, tubular fascial sheath found between the base of the skull and the root of the neck. It receives tissue contributions from all layers of the deep cervical fascia and encloses the common carotid and internal jugular vascular conduits and vagus nerve. After the bifurcation of the common carotid artery, the internal carotid branch will assume its position in the sheath. The vein is anterolateral to the artery, except at the base of the skull, where the vein lies posterior to the artery. The vagus nerve is between, and slightly posterior to, the blood vessels. The ansa cervicalis is on the anterior surface of the sheath in the cricoid plane. The sympathetic chain is in contact with the posterior surface of the sheath.
Root of the Neck
The root of the neck is the anatomical intersection between the thorax, neck, and axilla. The superior thoracic aperture, or thoracic inlet, and axillary (or cervicoaxillary) sheath create a pathway for the neurovascular
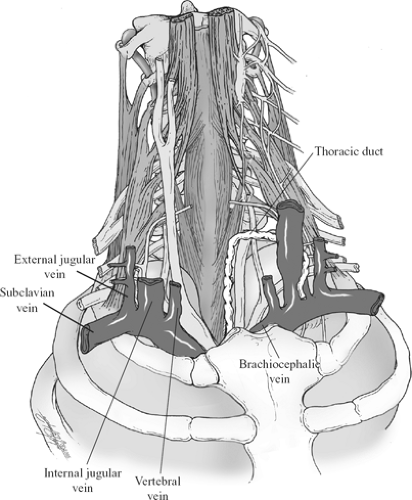
structures found in this area. Neck structures also contribute to the complexity of the anatomy in this important region. Passing between the clavicle and the first rib are nerves, arteries, and veins of the upper extremity. Narrowing of this costoclavicular canal can cause compression of these neurovascular structures. The thoracic inlet is created by the upper end of the manubrium anteriorly, the first rib and its costal cartilage laterally, and the first thoracic vertebra posteriorly. Structures passing through this area are medial or lateral in position. The esophagus and the trachea are medial as they enter the mediastinum. The thoracic duct lies just to the left of, and posterior to, the esophagus. In the root of the neck, at the level of C7, the duct passes laterally. It courses anterior to the left vertebral and left inferior thyroid arteries and posterior to the carotid sheath. It then travels anterior to the anterior scalene muscle. It is superficial to the prevertebral layer of the deep cervical fascia. The duct then descends anterior to the left subclavian artery and terminates at the lateral edge of the junction between the left internal jugular and the left subclavian veins (see Fig. 5).
structures found in this area. Neck structures also contribute to the complexity of the anatomy in this important region. Passing between the clavicle and the first rib are nerves, arteries, and veins of the upper extremity. Narrowing of this costoclavicular canal can cause compression of these neurovascular structures. The thoracic inlet is created by the upper end of the manubrium anteriorly, the first rib and its costal cartilage laterally, and the first thoracic vertebra posteriorly. Structures passing through this area are medial or lateral in position. The esophagus and the trachea are medial as they enter the mediastinum. The thoracic duct lies just to the left of, and posterior to, the esophagus. In the root of the neck, at the level of C7, the duct passes laterally. It courses anterior to the left vertebral and left inferior thyroid arteries and posterior to the carotid sheath. It then travels anterior to the anterior scalene muscle. It is superficial to the prevertebral layer of the deep cervical fascia. The duct then descends anterior to the left subclavian artery and terminates at the lateral edge of the junction between the left internal jugular and the left subclavian veins (see Fig. 5).
The equivalent of the thoracic duct on the right side of the root of the neck is called the right lymphatic duct. It is much smaller and may be represented by several small ducts. It receives lymph from the right hemithorax, right upper extremity, and right side of the head and the neck. Lymph from all other parts of the body is transported by the thoracic duct. The sympathetic chains are in contact with the head of the rib at this level. The recurrent laryngeal nerves, branches of the vagus (X) nerve, are also medial. The right recurrent laryngeal nerve arises in the root of the neck, loops around the right subclavian artery, and passes superomedially as it courses toward the tracheoesophageal groove. Its counterpart on the left arises in the mediastinum, loops around the aortic arch, and then ascends into the neck by way of the left tracheoesophageal groove. The right recurrent nerve, in the root of the neck, travels toward the right tracheoesophageal groove, but it may not yet have reached this protected position and is therefore more exposed to injury.
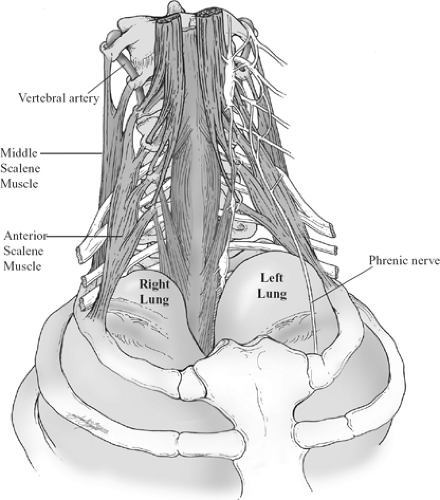
The apex of the cervical parietal pleura ascends to the neck of the first rib. The anterior end of the rib is lower than the posterior end; therefore, the apex of the lung can ascend out of the thorax into the root of the neck (Fig. 3). This ascension is most marked during deep inspiration and occupies the lateral portion of the superior thoracic inlet. This portion of the cervical pleura may extend above the superior edge of the clavicle. A tent-like thickening of the prevertebral fascia extends from the transverse mass of C7 to the first rib. It is called Sibson, or vertebropleural, fascia and provides some protection to the pleura when incisions are made in this area.
Lateral structures include the subclavian artery and subclavian vein and their branches, and nerve branches from the cervical and brachial plexuses. The cervical or apical area of the lung is also found in the lateral portion of the root of the neck. The first rib and the scalene muscles have important spatial relationships with the anatomy in this area.
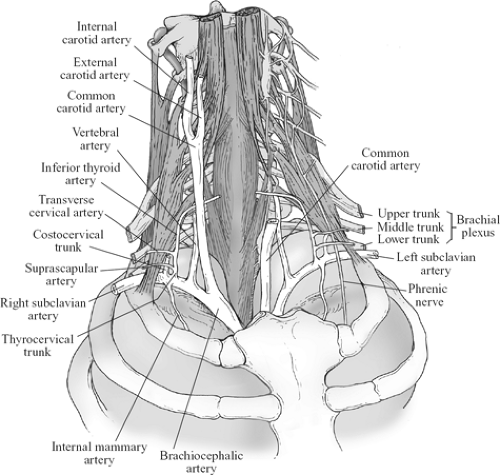
The brachiocephalic trunk is the first branch of the arch of the aorta (Fig. 4). It passes superolaterally and bifurcates at the level of the right sternoclavicular joint into the right common carotid and right subclavian arteries. The common carotid artery will pass superiorly on the right side of the neck in the carotid sheath. It will be discussed in more detail later in this chapter. The next branch of the arch of the aorta is the left common carotid artery. The last branch of the aortic arch is the left subclavian artery (Fig. 4). The anterior scalene muscle divides the subclavian artery into three segments. The first portion extends from the origin of the vessel to the medial edge of the anterior scalene muscle. The second part lies behind the muscle, and the third segment extends from the lateral edge of the muscle to the lower edge of the first rib. Most of the branches of the subclavian artery arise from the first portion. The first and largest branch is the vertebral artery. It arises from the superior edge of the parent vessel, ascends vertically, and enters a foramen in the transverse mass of the sixth cervical vertebra. The accompanying vein covers it.
The foramen is situated at the apex of a muscular triangle created by the longus coli muscle medially and the anterior scalene muscle laterally. This is referred to as the triangle of the vertebral artery. The second branch is the thyrocervical trunk, which also arises from the superior surface and has a short course before it divides into the following branches. The inferior thyroid artery passes superiorly, anterior to the anterior scalene muscle. The phrenic nerve is within the prevertebral fascia as it passes inferiorly on the anterior surface of this muscle. The inferior thyroid artery is superficial to the prevertebral fascia. At about the level of the apex of the triangle of the vertebral artery the inferior thyroid artery passes medially, coursing posterior to the carotid sheath but anterior to the vertebral artery, and enters the substance of the lateral lobe of the
thyroid gland. The transverse cervical and the suprascapular arteries are branches of the thyrocervical trunk that run transversely as they head for the lateral aspect of the neck. They cross the anterior scalene muscle and the phrenic nerve, but are superficial to the prevertebral fascia. The transverse cervical artery will divide into an ascending and descending branch when it reaches the margin of the trapezius muscle. The suprascapular artery will dip down below the clavicle after entering the posterior triangle, pass inferiorly, and contribute to the periscapular vasculature.
thyroid gland. The transverse cervical and the suprascapular arteries are branches of the thyrocervical trunk that run transversely as they head for the lateral aspect of the neck. They cross the anterior scalene muscle and the phrenic nerve, but are superficial to the prevertebral fascia. The transverse cervical artery will divide into an ascending and descending branch when it reaches the margin of the trapezius muscle. The suprascapular artery will dip down below the clavicle after entering the posterior triangle, pass inferiorly, and contribute to the periscapular vasculature.
The next branch originating from the superior aspect of the subclavian artery is the costocervical trunk (Fig. 4). It may arise from the second portion of the subclavian, and is therefore less at risk during surgical procedures. It arches over the cervical pleura and, when it reaches the neck of the first rib, divides into the deep cervical artery that passes up and supplies the muscles in the back of the neck and the supreme intercostal artery that creates the first and second posterior intercostal arteries. The first posterior intercostal vein that will enter the ipsilateral brachiocephalic vein, accompanies it.
The last branch of the subclavian artery is the internal thoracic or internal mammary artery. It arises from the inferior aspect of the subclavian artery across from the thyrocervical trunk. It passes inferomedially, courses posterior to the subclavian vein, and initially is in contact with the cervical pleura as it heads for the first costal cartilage. It then assumes its characteristic location parallel to the lateral edge of the sternum. The subclavian vein begins at the outer end of the first rib and then passes anterior to the anterior scalene muscle (Fig. 5). It receives the external jugular vein before reaching the medial edge of this muscle.
When the vein is medial to this muscle, it is joined by the internal jugular vein, forming the brachiocephalic vein. The left brachiocephalic vein will pass to the right, just inferior to the superior edge of the manubrium sternum, and join with its right counterpart behind the right first costal cartilage to create the superior vena cava. Each brachiocephalic vein will receive the corresponding vertebral vein. Each vagus nerve passes anterior to the related subclavian artery. The left nerve then passes posterior to the left brachiocephalic vein. The right nerve is posterolateral to the related brachiocephalic vein.
Anterior to this anatomical jungle is the thymus gland. It is largest during the childhood years, and then starts to regress with the onset of sexual maturation. The gland may extend from the thyroid cartilage above, to the pericardial sac below. Therefore, its superior portion is part of the medial, or anterior, aspect of the root of the neck. The gland is composed of two separate, asymmetrical lobes. The gland is contiguous with the large veins previously described. This explains why venous invasion is frequently seen with malignant disease of the gland.
The roots of the brachial plexus, C5 through T1, will create three trunks: an upper trunk (C5, C6), middle trunk (C7), and lower trunk (C8, T1) (Fig. 4). They will pass between the anterior and the middle scalene muscles on their way to the axilla. It is the lower trunk that is in direct contact with the upper surface of the first rib. It lies immediately posterior to the subclavian artery. The trunks pass through the posterior triangle. Each trunk will divide into an anterior and posterior division. These divisions, along with the accompanying subclavian vessels, will then pass through the costoclavicular space. The subclavian vein is the most medial of the structures passing through this space (Fig. 5). This vein is anteroinferior to the accompanying subclavian artery and can, therefore, be approached after the pulsations of the accompanying artery are palpated. The roots and trunks of the brachial plexus are within the prevertebral layer of the deep cervical fascia. As they head for the axilla, accompanied by the subclavian vessels, they drag some of this deep fascia along with them and create a protective tubular sheath for these neurovascular items called the cervicoaxillary, or axillary, sheath. These nerves and blood vessels, on their way to the axilla, pass under the insertion of the pectoralis minor muscle to the coracoid process of the scapula.
The Anatomy of the Root of the Neck Compression Syndromes
The root of the neck compression syndromes include the following:
Costoclavicular compression syndrome
Cervical rib syndrome
Anterior scalene compression syndrome
Pectoralis minor syndrome
If the space between the first rib and the clavicle should be decreased, there could be compression of the neurovascular structures traversing this area (Fig. 5). The subclavian vein is the most medial of the neurovascular structures passing through the costoclavicular space. The vein is in the narrowest portion of this space, and if additional narrowing occurs, venous outflow from the upper extremity may be impaired.
A cervical rib may present itself in several ways. It is frequently bilateral. It is an extension of the transverse mass of the seventh cervical vertebra and it may be a complete rib that articulates with the sternum. At times, it may fuse with the first rib or present as a fibrous band that attaches to the first rib. In some patients, it may have an anterior end that is free. The subclavian vessels and the brachial plexus, especially the lower trunk, will be affected adversely when they try to pass over this additional obstacle.
The anterior scalene compression syndrome results from spasm, or hypertrophy, of the anterior scalene muscle, with resultant constriction of the neurovascular elements as they pass through the scalene triangle. If the clinician treats this condition by transecting the anterior scalene muscle near its insertion, the position of the phrenic nerve and the subclavian vein, passing anterior to the muscle, must be remembered.
The term “thoracic outlet compression syndrome” is frequently used when defining some clinical conditions encountered in the root of the neck. Thoracic outlet is a misnomer when used to identify the clinical problems in this area. The true anatomical thoracic outlet is the area related to the respiratory diaphragm. Correct terms for these conditions would include superior thoracic aperture compression syndrome or cervicoaxillary compression syndrome.
All of these compression syndromes can result in neurologic deficits and/or arterial and venous circulatory problems in the upper extremity.
Clinical Anatomical Applications
Cervical incisions should be made parallel to the skin lines (lines of Langer) for good cosmesis. The neurovascular structures lie deep to the platysma muscle. The muscle must be carefully repaired for the best cosmetic result.
The middle cervical ganglion block: this sympathetic ganglion is found anterior to the transverse mass of the sixth cervical vertebra. At the level of the cricoid cartilage, retract the carotid sheath laterally and inject the medication after the needle strikes the lateral mass of the vertebra.
Control of bleeding may be possible if the common carotid artery is compressed against the transverse mass of the sixth cervical vertebra. This is the cricoid plane.
Carotid angiography: the common carotid artery is palpable in the carotid triangle. It is partially covered by the sternocleidomastoid muscle. Lateral retraction of the muscle will facilitate insertion of a catheter into the palpable artery.
Internal jugular vein catheterization: the internal jugular vein accompanies the common and internal carotid vessels. They all lie within the carotid sheath. The vein is anterolateral to the palpable artery.
The right internal jugular and right brachiocephalic veins, along with the superior vena cava, create a straight conduit to the right atrium and the inferior vena cava.
The subclavian vessels can be approached while passing through the costoclavicular space. The artery is palpable and the vein is situated anterior and medial to the artery. The vein is the most medial structure passing through the costoclavicular interval. A supraclavicular, or infraclavicular, technique can be used for catheterization.
The brachial plexus block approaches the nerves as they pass through the costoclavicular space. The subclavian artery is anterior to the branches of the plexus.
In cricothyroidotomy, the interior of the larynx is entered through the cricothyroid interval. The cricothyroid artery, a branch of the superior thyroid, pierces the cricothyroid ligament near the middle of the interval between the cricoid and the thyroid cartilages. A transverse incision, made close to the upper border of the cricoid arch, will avoid injury to this artery. The vocal ligaments are spared because they are superior to the point of entry.
For drainage of the retropharyngeal space, an incision is made at the level of the cricoid cartilage. The sternocleidomastoid muscle and carotid sheath are retracted posteriorly, and the lateral lobe of the thyroid gland is retracted anteriorly.
Using the external jugular vein as a conduit for central venous access, the external jugular vein is readily accessible because of its superficial position. It empties into the subclavian vein in the posterior triangle, but it may be difficult to negotiate the angle at the termination when attempting to introduce a device into the central portion of the circulatory system. Direct approach to the larger veins, right internal jugular or right subclavian, would eliminate this technical problem.
Triangles of the Neck
The layer-by-layer recreation of the neck anatomy now requires the addition of the carotid sheath with the vascular contents and their branches, the last four cranial nerves, and the viscera of the neck, which includes the thyroid and parathyroid glands, pharynx, and larynx. The superficial cervical plexus will also be outlined. The cervical lymphatic pathways will then be described, and finally the superficial venous circulation will be examined. This information is presented with a discussion of the triangles of the neck.
Anterior and Posterior Triangles
The sternocleidomastoid and trapezius muscles divide the neck into anterior and posterior triangles (Fig. 6; also see Fig. 13). The boundaries of the posterior triangle are the trapezius muscle posteriorly and the sternocleidomastoid muscle anteriorly. The middle third of the clavicle creates the inferior limit, and the apex of the triangle extends to the superior nuchal line. The triangle is spiral in shape. The inferior portion is anterior in the neck, but the apex is posterior. The anterior triangle includes the area between the anterior edges of the sternocleidomastoid muscles. The superior limit is the mandible and a line drawn from the angle of the mandible to the tip of the mastoid process. Two double-bellied muscles, omohyoid and digastric, subdivide the triangles. The inferior belly of the omohyoid muscle attaches to the superior transverse scapular ligament and a portion of the adjacent superior edge of the scapula. It passes superior to the clavicle and enters the lower portion of the posterior triangle. The intermediate tendon is in the cricoid plane, anterior to the carotid sheath, and is angulated by a fascial sling attached to the clavicle and the manubrium. The superior belly ascends to the hyoid bone.
The posterior triangle now consists of the large occipital and the smaller subclavian triangles. The digastric is the other double-bellied muscle that creates subdivisions of the anterior triangle. The posterior belly attaches just medial to the mastoid process. The intermediate tendon is tethered to the hyoid bone by a fold of deep cervical fascia. The stylohyoid muscle arises from the styloid process of the temporal bone and is in intimate contact with the anterior surface of the posterior belly of the digastric muscle. The tendon of insertion of the stylohyoid muscle to the hyoid bone is split and allows for passage of the intermediate tendon of the digastric muscle. The anterior triangle includes the submandibular and carotid triangles. They are separated from each other by median submental and muscular triangles.
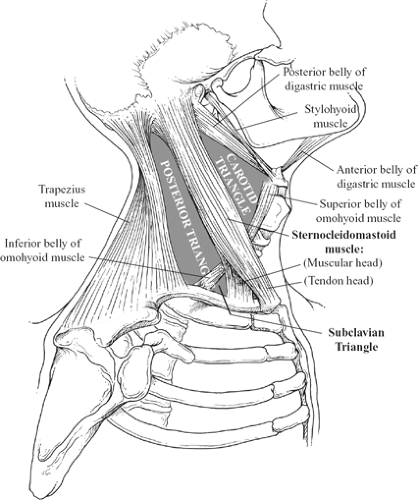 Fig. 6. Boundaries of the triangles of the neck (see also Fig. 14). |
The hyoid bone is a central structure in the neck. It is directly or indirectly attached to most of the muscular and membranous entities in the anterior triangle and in the floor of the mouth. If one considers the hyoid bone and the attached posterior belly of the digastric muscle, it is possible to divide the anterior triangle into suprahyoid and infrahyoid portions. The submandibular, or digastric triangles, and the submental triangle, are suprahyoid entities and are related to the floor of the mouth. They have been discussed in another chapter. The carotid and the muscular triangles are found in the infrahyoid portion of the anterior triangle.
Carotid Triangle
The muscular boundaries of the carotid triangle are the sternocleidomastoid muscle posteriorly, the posterior belly of the digastric muscle anterosuperiorly, and the superior belly of the omohyoid muscle anteroinferiorly (Fig. 7). The greater horn of the hyoid bone is part of the anterior and superior segment of the floor of this triangle. The hyoglossus and thyrohyoid muscles are attached to this portion of the hyoid bone, and are part of the anterior portion of the muscular floor. A small portion of the thyrohyoid membrane is found just behind the thyrohyoid muscle and makes up a small area of the floor. The middle and inferior pharyngeal constrictor muscles create the posterior section of the muscular floor of the carotid triangle. The longus capitis, a prevertebral muscle, also contributes to the posterior portion of the muscular floor of this triangle. The pretracheal layer of the deep cervical fascia creates the fascial carpet. The investing layer of the deep fascia creates a fascial roof.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree