Anatomy of the Cardiovascular System
HEART
Location of the Heart
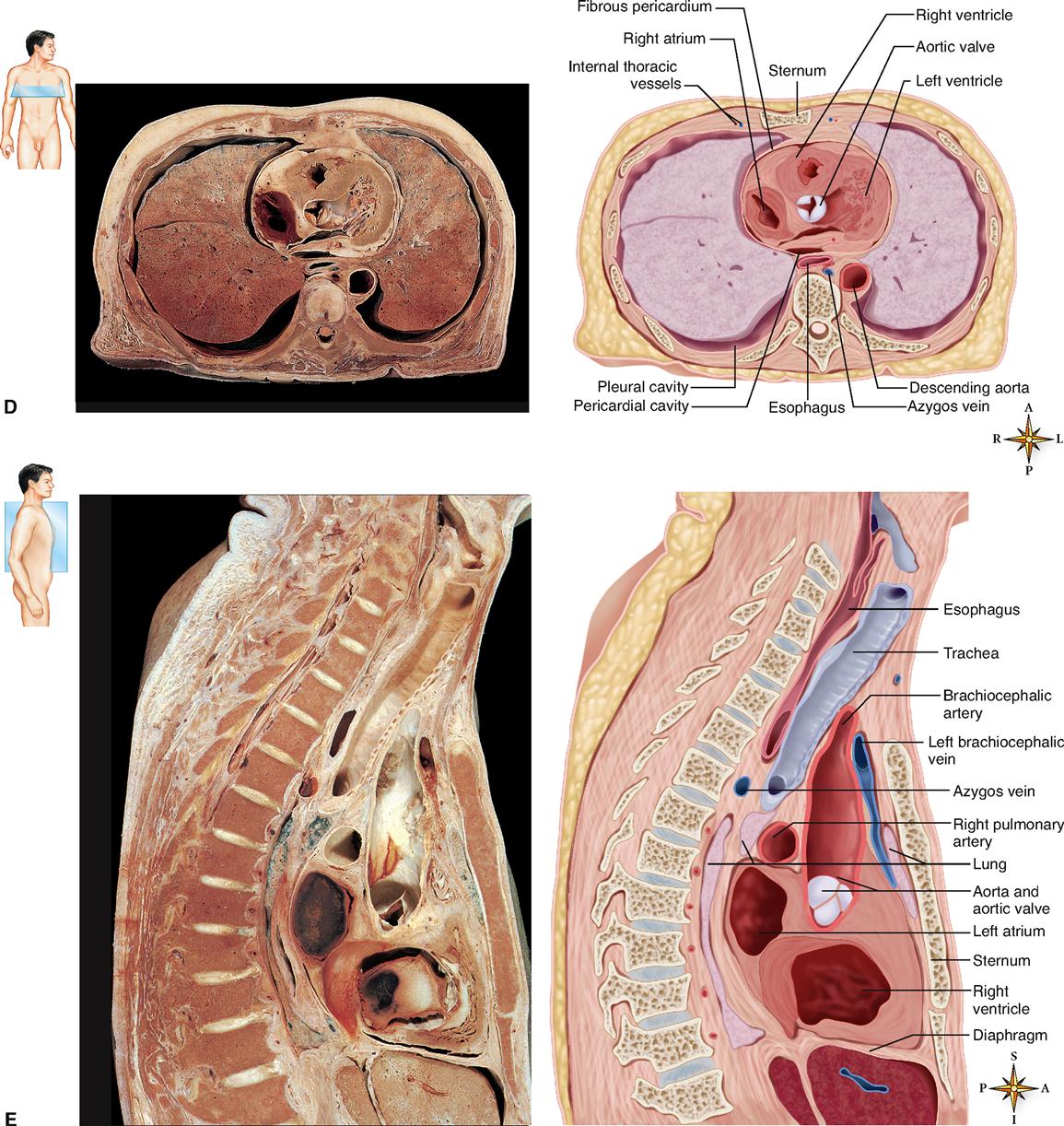
The human heart is a four-chambered muscular organ, shaped and sized roughly like a person’s closed fist (Figure 21-1). It lies in the mediastinum, or middle region of the thorax, just behind the body of the sternum between the points of attachment of the second through the sixth ribs. Approximately two thirds of the heart’s mass is to the left of the midline of the body, and one third is to the right (Figure 21-2).
Posteriorly the heart rests against the bodies of the fifth to the eighth thoracic vertebrae. Because of its placement between the sternum in front and the bodies of the thoracic vertebrae behind, it can be compressed by application of pressure to the lower portion of the body of the sternum using the heel of the hand (Figure 21-2, E). Rhythmic compression of the heart in this way can maintain blood flow in cases of cardiac arrest and, if combined with effective artificial respiration, the resulting procedure, called cardiopulmonary resuscitation (CPR), can be life saving.
The anatomical position of the heart in the thoracic cavity is shown in Figure 21-2. The lower border of the heart, which forms a blunt point known as the apex, lies on the diaphragm, pointing toward the left. To count the apical beat, one must place a stethoscope directly over the apex, that is, in the space between the fifth and sixth ribs (fifth intercostal space) on a line with the midpoint of the left clavicle.
The upper border of the heart, that is, its base, lies just below the second rib. The boundaries, which indicate its size, have considerable clinical importance, because a marked increase in heart size accompanies certain types of heart disease. Therefore, when diagnosing heart disorders, the physician charts the boundaries of the heart. The “normal” boundaries of the heart are, however, influenced by factors such as age, body build, and state of contraction.
Size and Shape of the Heart
At birth the heart is said to be transverse (wide) in type and appears large in proportion to the diameter of the chest cavity. In the infant, it is 1/130 of the total body weight compared with about 1/300 in the adult. Between puberty and 25 years of age the heart attains its adult shape and weight—about 310 grams is average for the male and 225 grams for the female.
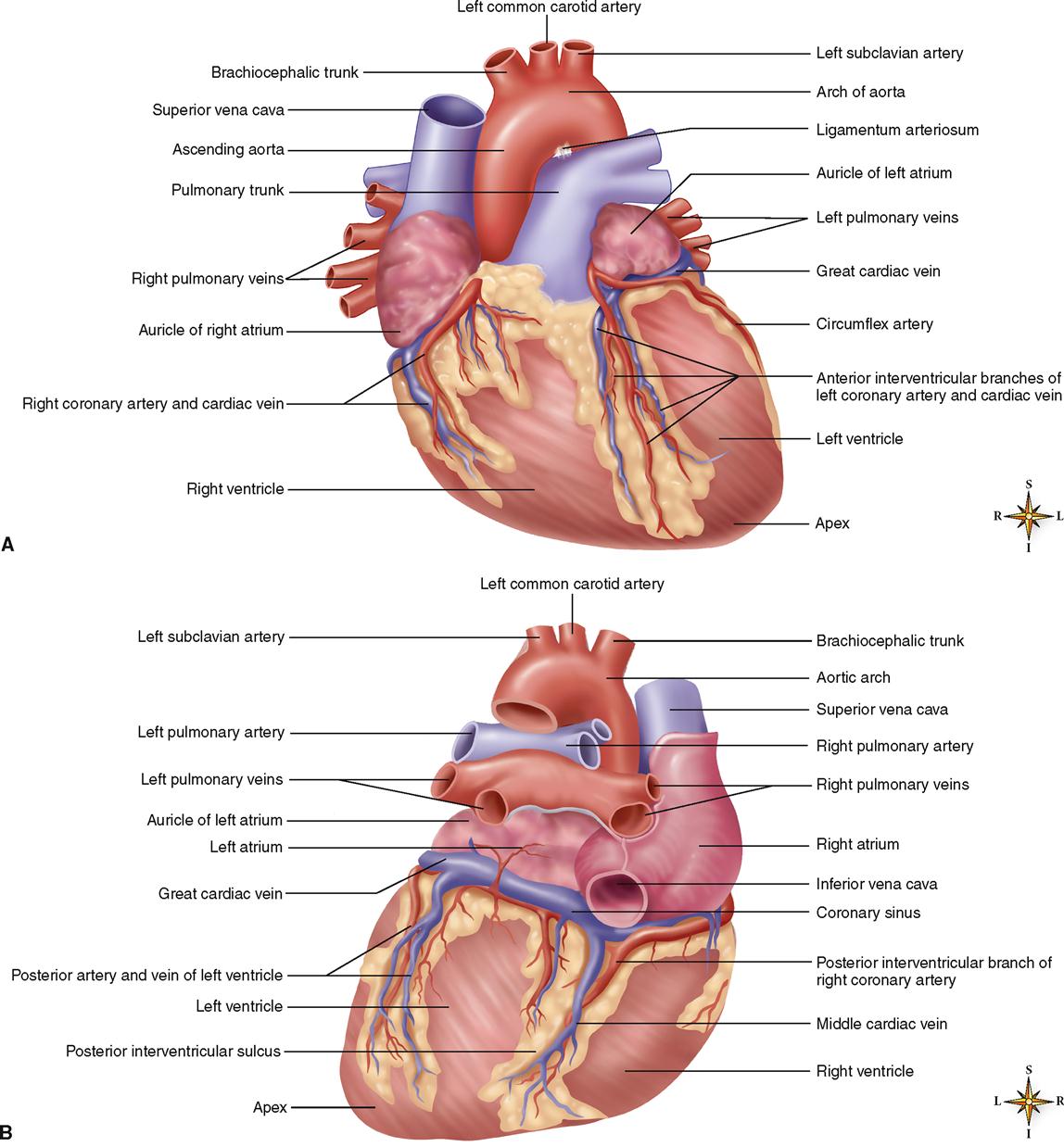
In the adult the shape of the heart tends to resemble that of the chest. In tall, thin individuals the heart is frequently described as elongated, whereas in short, stocky individuals it has greater width and is described as transverse. In individuals of average height and weight it is neither long nor transverse but somewhat intermediate between the two. Its approximate dimensions are 12 cm (4¾ inches) long, 9 cm (3½ inches) wide, and 6 cm (2½ inches) deep. Figure 21-3 shows details of the heart and great vessels in external views.
Coverings of the Heart
STRUCTURE OF THE HEART COVERINGS
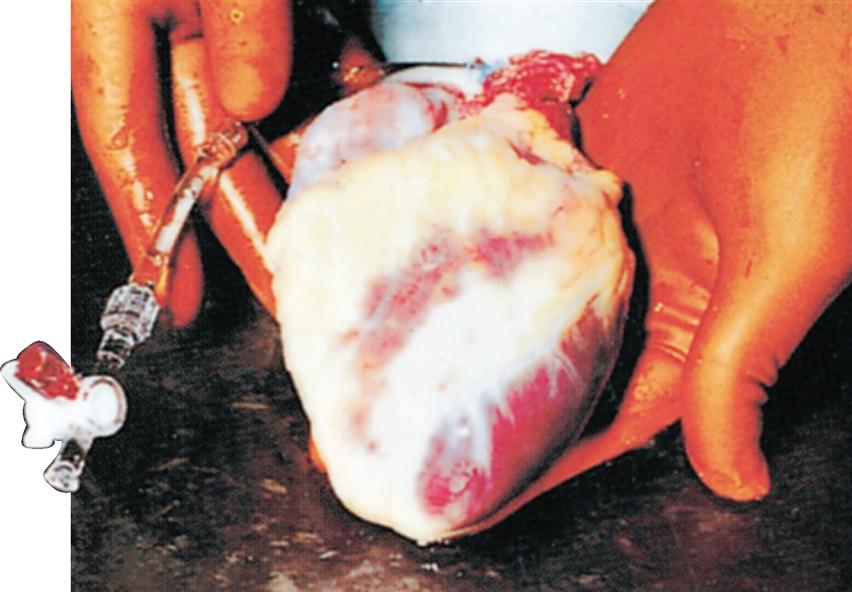
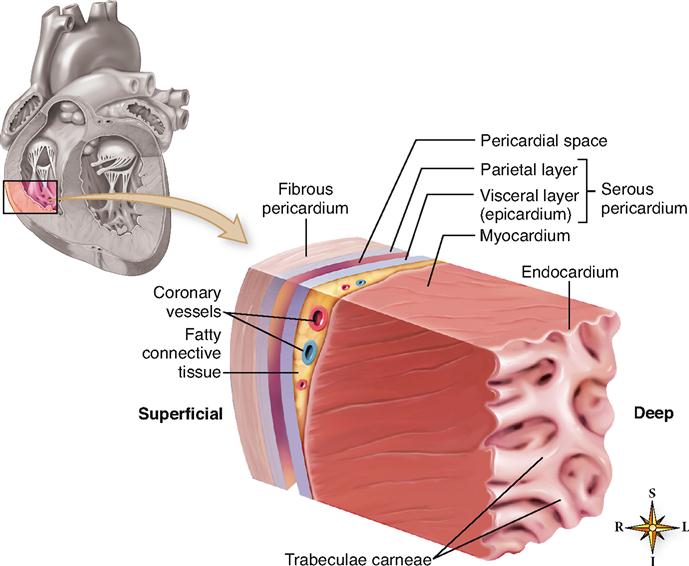
The heart has its own special covering, a loose-fitting inextensible sac called the pericardium. The pericardial sac, with the heart removed, can be seen in Figure 21-4. The pericardium consists of two parts: a fibrous portion and a serous portion (Figure 21-5). The sac itself is made of tough white fibrous tissue but is lined with smooth, moist serous membrane—the parietal layer of the serous pericardium. The same kind of membrane covers the entire outer surface of the heart. This covering layer is known as the visceral layer of the serous pericardium or the epicardium. The fibrous sac attaches to the large blood vessels emerging from the top of the heart but not to the heart itself (see Figure 21-4). Therefore it fits loosely around the heart, with a slight space between the visceral layer adhering to the heart and the parietal layer adhering to the inside of the fibrous sac. This space is called the pericardial space. It contains 10 to 15 ml of pericardial fluid, a lubricating fluid secreted by the serous membrane.
Fibrous pericardium—tough, loose-fitting, and inelastic sac around the heart
Serous pericardium—consisting of two layers
1. Parietal layer—lining inside the fibrous pericardium

FUNCTION OF THE HEART COVERINGS
The fibrous pericardial sac with its smooth, well-lubricated lining provides protection against friction. The heart moves easily in this loose-fitting jacket with no danger of irritation from friction between the two surfaces, as long as the serous pericardium remains normal and continues to produce lubricating serous fluid.
Structure of the Heart
WALL OF THE HEART
Three distinct layers of tissue make up the heart wall (see Figure 21-5) in both the atria and the ventricles: the epicardium, myocardium, and endocardium.
Epicardium
The outer layer of the heart wall is called the epicardium, a name that literally means “on the heart.” The epicardium is actually the visceral layer of the serous pericardium already described. In other words, the same structure has two different names: epicardium and serous pericardium.
Myocardium
The bulk of the heart wall is the thick, contractile, middle layer of specially constructed and arranged cardiac muscle cells called the myocardium. The minute structure of cardiac muscle has been described in Chapters 5 and 12. Review Table 6-7 on p. 152 for a brief overview of cardiac muscle.
Recall that cardiac muscle tissue is composed of many branching cells that are joined into a continuous mass by end-to-end junctions called intercalated disks (see Figure 6-35 on p. 153). Because each intercalated disk includes many gap junctions, large areas of cardiac muscle are electrically coupled into a single functional unit called a syncytium (meaning “joined cells”). Figure 13-23 on p. 400 shows how such electrical connections work. Because they form an electrically coupled syncytium, cardiac muscle cells can pass an action potential from fiber to fiber along a large area of the heart wall—thus stimulating contraction in each muscle fiber of the syncytium.
Another advantage of the linked structure of myocardial cells is that the cardiac fibers form a continuous sheet of muscle that wraps entirely around the cavities within the heart. Thus the encircling myocardium can compress the heart cavities, and the blood within them, with great force.
Recall also that cardiac muscles are autorhythmic, meaning that they can contract on their own in a slow, steady rhythm. As we explained in Chapter 12, cardiac muscle cells cannot summate contractions to produce tetanus and thus do not fatigue—a useful characteristic for muscle tissue that must maintain a continuous cycle of alternating contraction and relaxation for the entire span of life. Because the muscular myocardium can contract powerfully and rhythmically, without fatigue, the heart is an efficient and dependable pump for blood.
If the myocardium is damaged, as it may be in a “heart attack” or myocardial infarction (MI), then it will not pump as efficiently—which may quickly lead to death if the damage is severe. Such damage can be diagnosed by analyzing cardiac marker molecules released into the blood by damaged cardiac muscle fibers (Box 21-1).
Endocardium
The lining of the interior of the myocardial wall is a delicate layer known as the endocardium. The endocardium is made of a type of tissue called endothelial tissue, or simply endothelium. Endothelium lines the heart (where it is called the endocardium) and continues on to line all of the blood vessels. Endothelium is a specialized type of simple squamous epithelium.
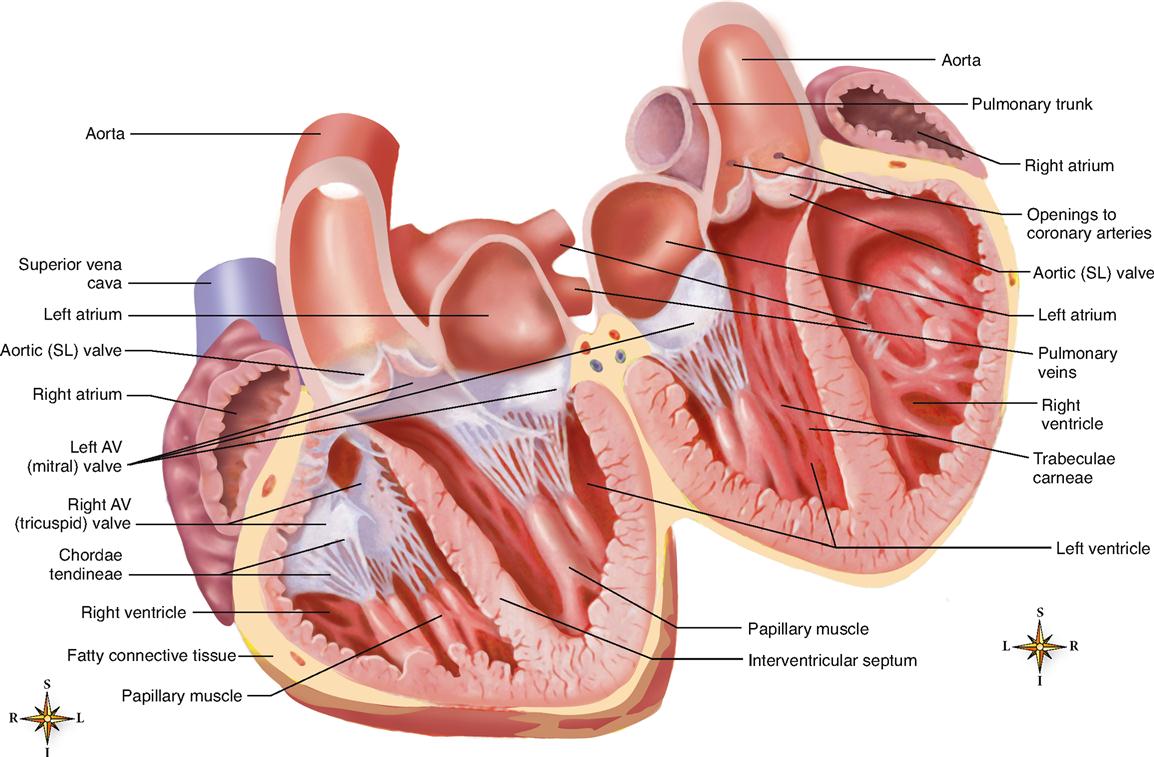
Note in Figure 21-5 that the endocardium covers beamlike projections of myocardial tissue. These muscular projections are called trabeculae carneae (meaning “fleshy beams”) and help to add force to the inward contraction of the heart wall.
Inward folds or pockets formed by the endocardium and supporting connective tissue make up the flaps or cusps of the major heart valves. These valves ensure the one-way flow of blood through the chambers of the heart, thus enabling the heart to act as a pump.
CHAMBERS OF THE HEART
The interior of the heart is divided into four cavities, or heart chambers (Figure 21-6). The two upper chambers are called atria (singular, atrium), and the two lower chambers are called ventricles. The left chambers are separated from the right chambers by an extension of the heart wall called the septum.
Atria
The two superior chambers of the heart—the atria—are separated into left and right chambers by the interatrial septum. Atria are often called the “receiving chambers” because they receive blood from vessels called veins. Veins are the large blood vessels that return blood from various tissues to the heart so that the blood can be pumped out to tissues again.
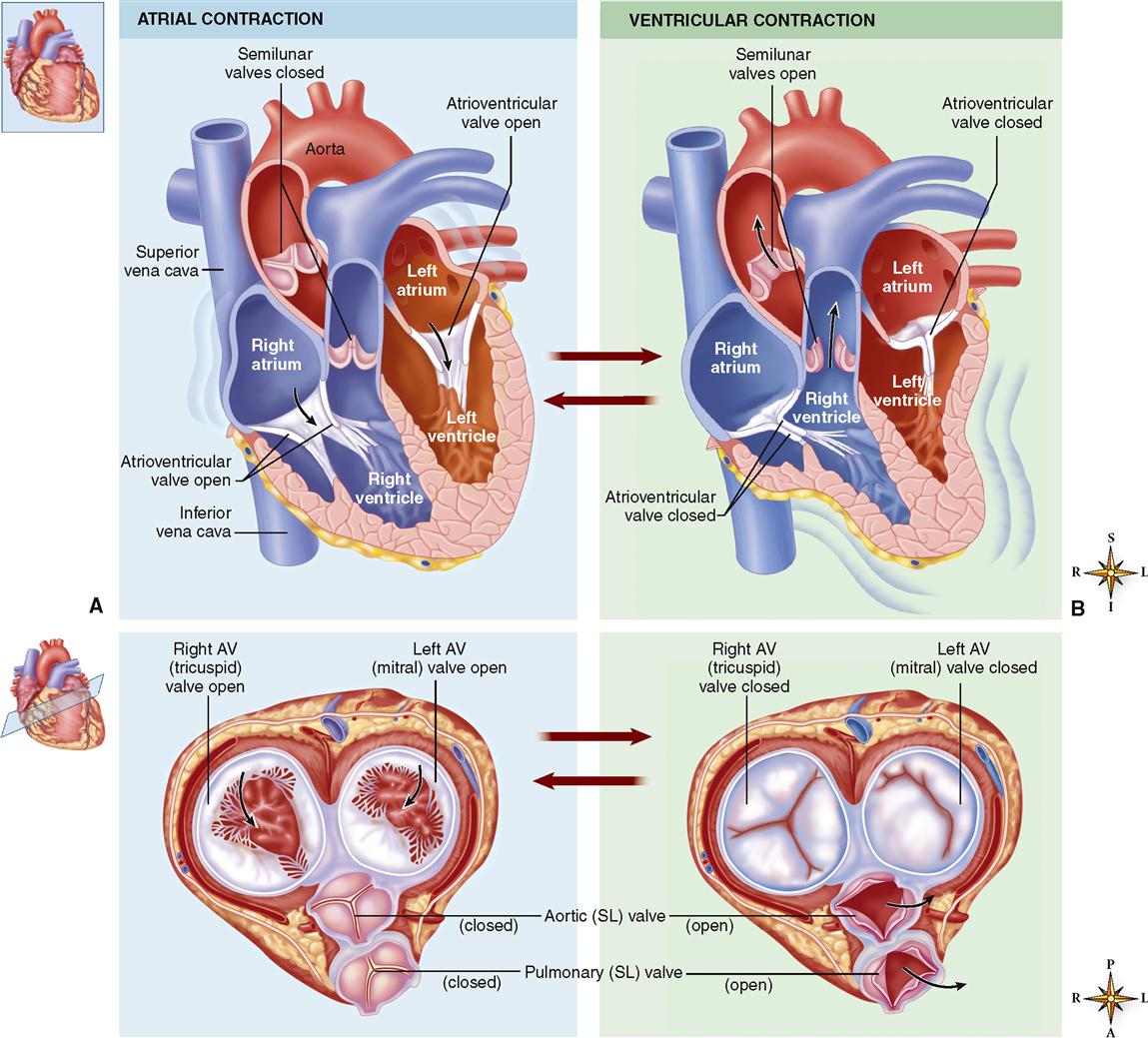
Figure 21-7 shows how the atria alternately relax and contract to receive blood, then push it into the lower chambers. Because the atria need not generate great pressure to move blood such a small distance, the myocardial wall of each atrium is not very thick.
If you look at Figures 21-2, C, and 21-3, A, you will notice that part of each atrium is labeled as an auricle. The term auricle (meaning “little ear”) refers to the earlike flap protruding from each atrium. Thus the auricles are part of the atria. The terms auricles and atria should not be used synonymously.
Ventricles
The ventricles are the two lower chambers of the heart. The ventricles are separated into left and right chambers by the interventricular septum. Because the ventricles receive blood from the atria and pump blood out of the heart into arteries, the ventricles are considered to be the primary “pumping chambers” of the heart.
Because more force is needed to pump blood a farther distance from the ventricles than from the atria, the myocardium of each ventricle is thicker than the myocardium of either atrium. The myocardium of the left ventricle is thicker than that of the right ventricle because the left ventricle pushes blood through most vessels of the body, whereas the right ventricle pushes blood only through the nearby pulmonary vessels that serve the gas exchange tissues of the lungs.
The pumping action of the heart chambers is summarized in Figure 21-7 and described further in Chapter 22.
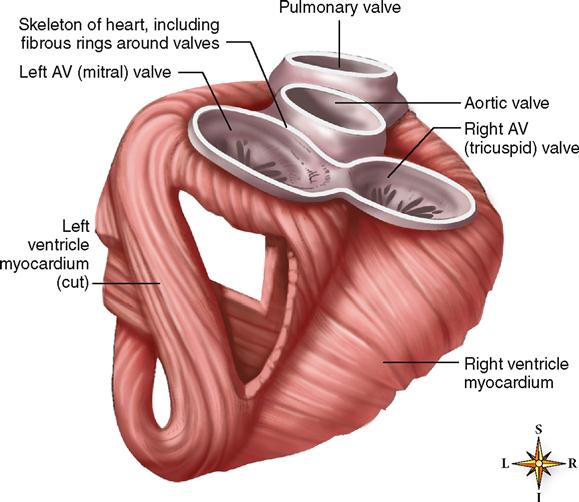
VALVES OF THE HEART
The heart valves are structures that permit the flow of blood in one direction only—allowing the heart to act as a pump that forces the continuous flow of blood in one direction.
Four valves are of importance to the normal functioning of the heart (Figure 21-8; see Figure 21-7). Because they guard the openings between the atria and the ventricles, two of the valves are called the atrioventricular (AV) valves. The atrioventricular valves have pointed leaflets or flaps called cusps and are therefore also called cuspid valves. The other two heart valves, the heart’s semilunar (SL) valves, are located where the trunk of the pulmonary artery joins the right ventricle (pulmonary valve) and where the aorta joins the left ventricle (aortic valve).
Atrioventricular Valves
The atrioventricular valve regulating flow through the right atrioventricular opening consists of three flaps (cusps) of endocardium. The free edge of each flap is anchored to the papillary muscles of the right ventricle by several tendinous cords that are more often called chordae tendineae.
Because the right atrioventricular valve has three flaps or cusps, it is also called the tricuspid valve. The valve that guards the left atrioventricular opening is similar in structure to the right atrioventricular valve, except that it has only two flaps and is therefore also called the bicuspid valve. Most commonly, however, the left AV valve is called the mitral valve—a name it gets from its resemblance to the miter, a double-cusp hat worn by bishops.
The construction of both atrioventricular valves allows blood to flow from the atria into the ventricles but prevents it from flowing back up into the atria from the ventricles. When ventricles are relaxed, blood can flow through the AV valve from the atrium by simply pushing the flimsy valve cusps aside, into the ventricle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree