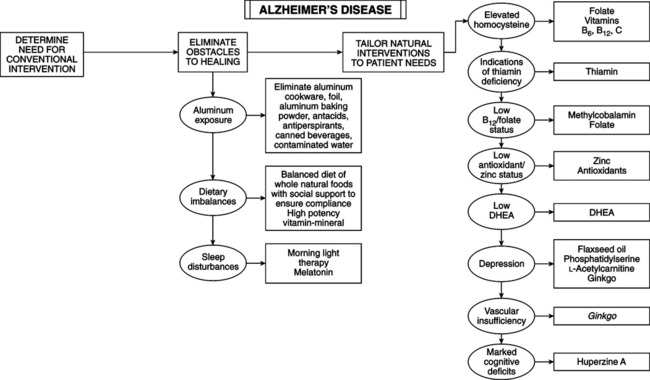
• Progressive mental deterioration, loss of memory and cognitive functions, inability to carry out activities of daily life • Characteristic symmetrical, usually diffuse, EEG pattern • Diagnosis usually made by exclusion • Definitive diagnosis can be made only by postmortem biopsy of brain, demonstrating atrophy, senile plaques, and neurofibrillary tangles • Lifestyle factors: diet—excess saturated or trans fatty acids may predispose neurons to aluminum-induced toxicity. Sleep—abnormal sleep-wake cycles and decreased morning light exposure (see melatonin, later). • Other factors: traumatic head injury; long-term exposure to aluminum, silicon, environmental neurotoxins, and free radicals; increased oxidative damage. • Homocysteine: increased plasma (and perhaps urine) homocysteine is a strong, independent risk factor for dementia and AD, just as it is for atherosclerosis. Plasma level greater than 14 μmol/L nearly doubles risk of AD. Control homocysteine with folate and vitamins B12, B6, and C. • Aluminum (AL): concentrated in neurofibrillary tangles and significantly contributes to AD; strong affinity for and cofactor with paired helical filament tau (PHFt) involved in forming neurofibrillary tangles. AL selectively binds to PHFt, induces PHFt aggregation, and retards brain’s ability to break down PHFt. Long-term exposure of animals to ecologic doses of AL induces ghostlike neurons with cytoplasmic and nuclear vacuolations, with AL deposits; neuritic plaques in hippocampus; amyloid deposits in cerebrovasculature; behavorial changes reminiscent of AD. Brain and serum AL levels increase with age as AD incidence increases with age. Patients with AD have much higher AL than normal people and patients with other dementias (ETOH, atherosclerosis, stroke). Efforts to remove AL help but probably are too late, after disease is well established. Even in those without mental disease, elevated AL is linked with poorer mental function. Sources of AL are water supply (immediately enters brain tissue), food, antacids, anti-perspirants. • Diagnostic process: exclude other possible diagnoses. — Step 1: diagnose dementia accurately. (10%-50% error rate when diagnosis is based only on first evaluation. Avoid misdiagnosing pseudodementing functional illness. Depression mimics dementia in the elderly. Causes and Mechanisms of Development of Senile Dementia
Alzheimer’s Disease
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
Etiology
DIAGNOSTIC CONSIDERATIONS
Etiology
Pathogenesis
Degenerative Etiology
Disturbances of gene expression and thus of protein metabolism
Altered genetic code
Disturbance of the synthesis of specific proteins
Alzheimer’s disease
Reduction in acetylcholine synthesis resulting from decreased ChAc activity
Huntington’s chorea
Disturbance of the GABAergic system
Idiopathic dementia, localized form
Decline in cognitive function
Parkinson’s disease
Reduction in dopamine turnover
Pick’s disease
Reduction in cholinergic activity
Loss of neuronal redundancy
Disturbance of cerebral metabolism after infection or trauma; reduction in cholinergic activity caused by loss of neurons and synapses
Cerebrovascular disease
Chronic meningitis
Tuberculosis, mycotic
Encephalopathy after head injury (boxers)
Viral encephalopathy
Encephalomyelitis
Epileptic dementia
Etiology
Pathogenesis
Nutritive Etiology
Chronic alcoholism
Diabetes mellitus
Disturbances of electrolyte metabolism
Hypoglycemia
Insulin, starvation
Hyponatremia
Diuretics
Hypothyroidism
Korsakoff syndrome
Thiamine transketolase deficiency
Nicotinamide deficiency
Vitamin B deficiency
Disturbances of energy formation
Toxic Etiology
Addiction to barbituates, psychotropic drugs, etc.
Chronic CO intoxication
Chronic CO2 intoxication
Mycotoxins
Renal/hepatic encephalopathy
Vincristine intoxication
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Alzheimer’s Disease
