High-Yield Terms to Learn
Alcoholism Compulsive use of ethanol Alcohol withdrawal syndrome The characteristic syndrome of insomnia, tremor, agitation, seizures, and autonomic instability engendered by deprivation in an individual who is physically dependent on ethanol Delirium tremens (DTs) Severe form of alcohol withdrawal whose main symptoms are sweating, tremor, confusion, and hallucinations Fetal alcohol syndrome A syndrome of craniofacial dysmorphia, heart defects, and mental retardation caused by the teratogenic effects of ethanol consumption during pregnancy Wernicke-Korsakoff syndrome A syndrome of ataxia, confusion, and paralysis of the extraocular muscles that is associated with chronic alcoholism and thiamine deficiency
Ethanol
Pharmacokinetics
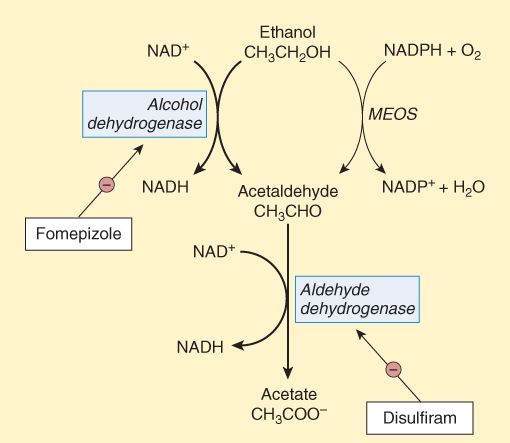
After ingestion, ethanol is rapidly and completely absorbed; the drug is then distributed to most body tissues, and its volume of distribution is equivalent to that of total body water (0.5-0.7 L/kg). Two enzyme systems metabolize ethanol to acetaldehyde (Figure 23-1).
FIGURE 23-1
Metabolism of ethanol by alcohol dehydrogenase (ADH) and the microsomal ethanol-oxidizing system (MEOS). Alcohol dehydrogenase and aldehyde dehydrogenase are inhibited by fomepizole and disulfiram, respectively.
(Reproduced, with permission, from Katzung BG, Masters SB, Trevor AT, editors: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 23-1.)
Alcohol Dehydrogenase (ADH)
This cytosolic, NAD+-dependent enzyme, found mainly in the liver and gut, accounts for the metabolism of low to moderate doses of ethanol. Because of the limited supply of the coenzyme NAD+, the reaction has zero-order kinetics, resulting in a fixed capacity for ethanol metabolism of 7-10 g/h. Gastrointestinal metabolism of ethanol is lower in women than in men.
Microsomal Ethanol-Oxidizing System (MEOS)
At blood ethanol levels higher than 100 mg/dL, the liver microsomal mixed function oxidase system that catalyzes most phase I drug-metabolizing reactions (see Chapter 2) contributes significantly to ethanol metabolism (Figure 23-1). Chronic ethanol consumption induces cytochrome P450 enzyme synthesis and MEOS activity; this increase may be partially responsible for the development of tolerance to ethanol. The primary isoform of cytochrome P450 induced by ethanol—2E1 (see Table 4-3)—converts acetaminophen to a hepatotoxic metabolite.
Acetaldehyde formed from the oxidation of ethanol by either ADH or MEOS is rapidly metabolized to acetate by aldehyde dehydrogenase, a mitochondrial enzyme found in the liver and many other tissues. Aldehyde dehydrogenase is inhibited by disulfiram and other drugs, including metronidazole, oral hypoglycemics, and some cephalosporins. Some individuals, primarily of Asian descent, have genetic deficiency of aldehyde dehydrogenase. After consumption of even small quantities of ethanol, these persons experience nausea and a flushing reaction from accumulation of acetaldehyde.
Acute Effects
CNS
The major acute effects of ethanol on the CNS are sedation, loss of inhibition, impaired judgment, slurred speech, and ataxia. In nontolerant persons, impairment of driving ability is thought to occur at ethanol blood levels between 60 and 80 mg/dL. Blood levels of 120 to 160 mg/dL are usually associated with gross drunkenness. Levels greater than 300 mg/dL may lead to loss of consciousness, anesthesia, and coma sometimes with fatal respiratory and cardiovascular depression. Blood levels higher than 500 mg/dL are usually lethal. Chronic alcoholics who are tolerant to the effects of ethanol can function almost normally at much higher blood concentrations than occasional drinkers. Additive CNS depression occurs with concomitant ingestion of ethanol and a wide variety of CNS depressants, including sedative-hypnotics, opioid agonists, and many drugs that block muscarinic and H1 histamine receptors. The molecular mechanisms underlying the complex CNS effects of ethanol are not fully understood. Specific receptors for ethanol have not been identified. Rather, ethanol appears to modulate the function of a number of signaling proteins. It facilitates the action of GABA at GABAA receptors, inhibits the ability of glutamate to activate NMDA (N-methyl-D-aspartate) receptors, and modifies the activities of adenylyl cyclase, phospho-lipase C, and ion channels. It has been suggested that alcohol “blackouts” may result from interference with NMDA receptors.
Other Organ Systems
Ethanol, even at relatively low blood concentrations, significantly depresses the heart. Vascular smooth muscle is relaxed, which leads to vasodilation, sometimes with marked hypothermia. Ethanol relaxes uterine smooth muscle.
Chronic Effects
Tolerance and Dependence
Tolerance occurs mainly as a result of CNS adaptation and to a lesser extent by an increased rate of ethanol metabolism. There is cross-tolerance to sedative-hypnotic drugs that facilitate GABA activity (eg, benzodiazepines and barbiturates). Both psychological and physical dependence are marked.
Liver
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree