Aggressive Epidermotropic CD8+ Cytotoxic T-cell Lymphoma
Aaron Auerbach, MD, PhD
Key Facts
Terminology
Provisional diagnosis in the 2008 WHO, T-cell lymphoma consisting of CD8(+) cytotoxic αβ T cells in epidermis, exhibiting aggressive clinical behavior
Previously included in cases of peripheral T-cell lymphoma, not otherwise specified
Often separated from other CD8(+) lymphomas based on clinical behavior
Clinical Issues
Rare
Often disseminated tumors, nodules, and papules with ulceration/necrosis
Rapid spread to lungs, testes, brain, and oral cavity
Often spares lymph nodes
Often treated with multiagent chemotherapy
Aggressive clinical course
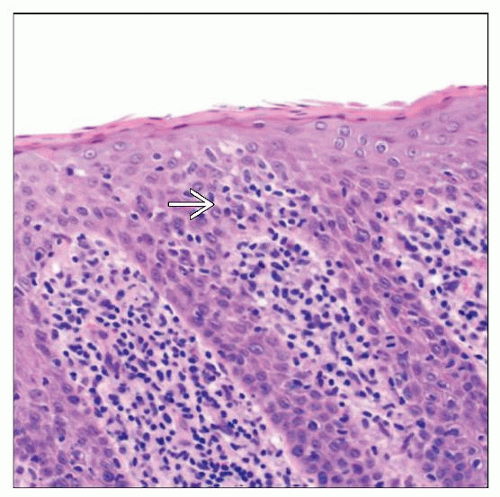
Microscopic Pathology
T-cell infiltrate in dermis with epidermotropism
Small to medium-sized T cells with moderate to marked atypia
Ancillary Tests
CD3(+), CD2(+), βF1(+), CD4(−), CD8(+), LMP1(−), CD15(-/+), CD56(+/-)
Clonal for T-cell receptor gene gamma rearrangement
Top Differential Diagnoses
Mycosis fungoides
Is rarely CD8(+), but progression to tumor stage often takes years
Lymphomatoid papulosis
More banal clinical course with papules that spontaneously regress
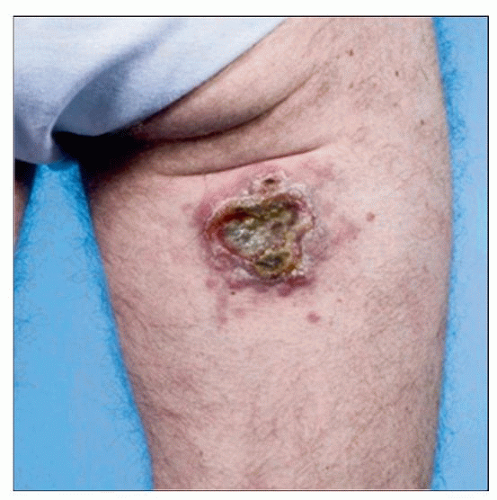 This is a clinical photograph of a large tumor on the posterior leg of a person with AECTCL. As is typical of this disease, the lesion is extensively ulcerated. (Courtesy R. Willemze, MD.) |
TERMINOLOGY
Abbreviations
Aggressive epidermotropic cytotoxic T-cell lymphoma (AECTCL)
Synonyms
Primary cutaneous aggressive epidermotropic cytotoxic T-cell lymphoma
Definitions
T-cell lymphoma consisting of CD8(+) cytotoxic αβ T cells prominently involving the epidermis and exhibiting aggressive clinical behavior
Provisional entity in the 2008 WHO Classification of Hematopoietic and Lymphoid Tissues
Previously included in cases of peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS)
Often separated from other CD8(+) lymphomas based on clinical behavior
CLINICAL ISSUES
Epidemiology
Incidence
Rare
< 1% of cutaneous T-cell lymphomas
Age
Adults
Median age: 53
Gender
Male:female = 1.4:1.0
Presentation
Skin lesions
Often tumors, nodules, and papules
Less often patches or plaques
Usually ulceration &/or necrosis
Often widespread disseminated lesions
Rapid extracutaneous spread
Fairly frequent
Lungs, testes, brain, and oral cavity involved
Lymph nodes are usually spared
Treatment
Adjuvant therapy
Often multiagent chemotherapy
Prognosis
Aggressive clinical course
32-month median survival
No difference in prognosis if tumor cells are smaller or larger
1 study suggests that CD2(−)/CD7(+) cases have worse prognosis
MICROSCOPIC PATHOLOGY
Histologic Features
T-cell infiltrate in dermis
Can involve superficial dermis or deeper tissues
Sometimes angiocentric
Sometimes lichenoid
Destroys adnexa
Epidermotropism
Can be pagetoid spread with linear colonization of basal epidermis
Epidermis
Ulceration, necrosis, or blister common
Can be acanthotic or atrophic
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree