2 Ageing and disease
Over the last 100 years the proportion of people in the UK aged >65 yrs has risen from 5% to 16%, and is projected to increase steadily to 24% in 2061. This increase has been particularly apparent in people aged >85. Life expectancy in the developed world is now substantial, even in old age. Although the proportion of the population aged >65 is greater in developed countries, most older people live in the developing world. Two-thirds of the world population of people aged >65 live in developing countries at present, and this is projected to rise to 75% in 2025.
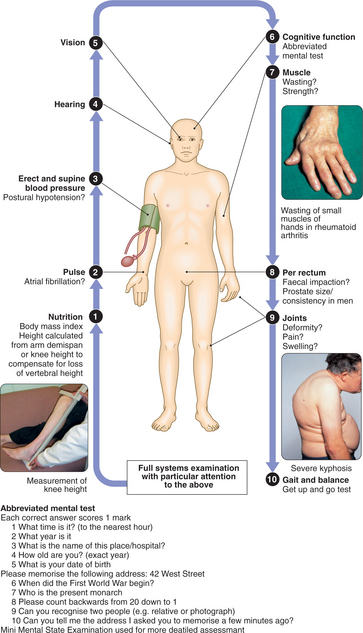
Geriatric medicine applies the knowledge and clinical skills of the organ-based specialties to a complex group: frail older people. This group is defined by the reduction in physiological capacity that makes them more susceptible to disease and mortality. As a result they frequently have multiple pathology, and illness often presents in atypical ways with confusion, falls, or loss of mobility and day-to-day functioning. Frail older people are also prone to adverse drug reactions, partly because of polypharmacy and partly because of age-related changes in responses to drugs and their elimination. Disability is common in old age but patients’ function can often be improved by the interventions of the multidis-ciplinary team (Box 2.1), which includes nurses as well as physiotherapy, occupational and speech therapy, and medical staff.
2.1 MULTIDISCIPLINARY TEAM (MDT) AND FUNCTIONAL ASSESSMENT ![]()
| Team member | Activity assessed and promoted |
|---|---|
| Physiotherapist | Mobility, balance and upper limb function |
| Occupational therapist | Activities of daily living, e.g. dressing, cooking; (assessment of home environment) |
| Dietitian | Nutrition |
| Speech and language therapist | Communication and swallowing |
| Social worker | Care needs |
| Nurse | Motivation and initiation of activities; feeding; continence |
PRESENTING PROBLEMS
The approach to most presenting problems in old age can be summarised as follows:
FALLS
Falls and unsteadiness are very common in older people. Although only 10–15% of falls result in serious injury, they are the principal cause of fractured neck of femur in this age group. Falls also lead to loss of confidence and fear, and are frequently the ‘final straw’ that makes an older person decide to move to institutional care. The approach to the patient varies according to the underlying cause of falls, as follows.
Blackouts
A proportion of older people who ‘fall’ have in fact had a syncopal episode. It is important to ask about loss of consciousness and, if this is a possibility, to perform appropriate investigations (pp. 211 and 617). Recent research suggests that in small numbers of patients, carotid sinus hypersensitivity (p. 212) may be the cause of otherwise unexplained falls.
Acute illness
Falling is one of the classical atypical presentations of acute illness in the frail. The reduced reserves in older people’s integrative neurological function mean that they are less able to maintain their balance when challenged by an acute illness. Suspicion should be especially high when falls have occurred suddenly over a period of a few days. Common underlying illnesses include infection, stroke, metabolic disturbance and heart failure. Thorough examination and investigation are required to identify these (Box 2.2). It is also important to establish whether any drug has been started recently, as this may precipitate falls. Once an underlying acute illness has been treated, falls may no longer be a problem.
Multiple risk factors
Many patients, especially those with recurrent falls, are frail with multiple medical problems and chronic disabilities. Their tendency to fall is associated with risk factors that have been well established from prospective studies (Box 2.3). The annual risk of falling increases linearly with the number of risk factors present: from 8% with no risk factors to 78% in those with four or more. Obviously, such patients may present with a fall resulting from an acute illness or syncope as above, but they will remain at risk of further falls even when the acute illness has resolved.