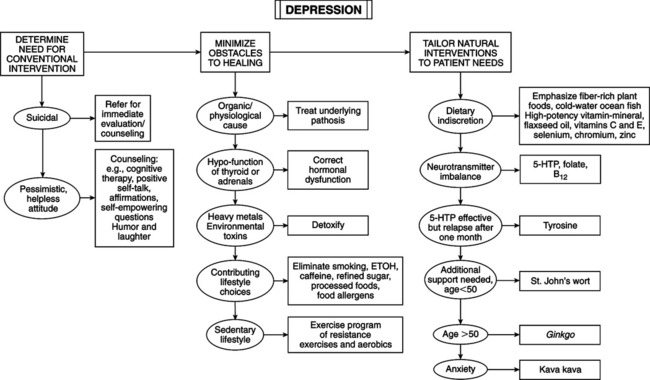
Depression (major or unipolar depression)—DSM-IV criteria: • Poor appetite with weight loss or increased appetite with weight gain • Physical hyperactivity or inactivity • Loss of interest or pleasure in usual activities, decrease in sexual drive • Loss of energy and feelings of fatigue • Feelings of worthlessness, self-reproach, or inappropriate guilt • Diminished ability to think or concentrate • Low self-esteem, lack of self-confidence • Pessimism, hopelessness, despair • Lack of interest in ordinary pleasures and activities • Withdrawal from social activities • Guilt, ruminating about past • Irritability, excessive anger • Eight factors modify functional state of brain and affect mood and behavior: genetic inheritance; age of neuronal development (age-specific variability); functional plasticity of brain during development; motivational state affected by biologic drives, channeling behavior toward goals by priorities or prejudicing context of incoming information; memory-stored information and processing strategies; environment that adjusts incoming input according to momentary significance; brain disease or lesion causing aberrant function; metabolic or hormonal system or biochemical environment of central nervous system (CNS). • Five theoretical models: “aggression turned inward” (apparent in many cases but no substantial proof); “loss model” (depression = reaction to loss of person, thing, status, self-esteem, or habit pattern); “interpersonal relationship” (depressed person uses depression to control other people, including doctors, by pouting, silence, or ignoring something or someone); “learned helplessness” (habitual feelings of pessimism and hopelessness); “biogenic amine” hypothesis (biochemical derangement of biogenic amines). Learned helplessness model (Martin Seligman, PhD) is most useful. • Biogenic amine model: dominant medical conception of depression. Counseling is valuable, especially with clear psychological etiology. • Learned helplessness (Seligman): Animals and human beings can be experimentally conditioned to feel and act helpless. Animals conditioned to be helpless have alteration of brain monoamine content; teaching them how to gain environmental control normalizes brain chemistry. Altered brain monoamines in animals with learned helplessness mirror altered brain monoamine biochemistry in human beings during depression. This model revolutionized psychopharmacology; animals conditioned to be helpless and then given antidepressant drugs unlearn helplessness and exercise control over environment. Antidepressants restore monoamine balance and, thereby, alter behavior. Helping patients gain control over their lives produces greater brain biochemical changes than drugs. Powerful technique—teach optimism. Determining factor for person’s reaction to uncontrollable events = “explanatory style” (how patient explains events to self). Optimistic people are immune to helplessness and depression; they have positive, optimistic explanatory style. Pessimists are susceptible to depression when “bad” things happen; they have negative, fatalistic explanatory style. Direct correlation between level of optimism and risk for depression and other illnesses. • Counseling: most merit and support in medical literature—cognitive therapy—as effective as antidepressants for moderate depression with lower rate of relapse. Patient is taught new skills to change the way he or she consciously thinks about failure, defeat, loss, and helplessness. Five basic tactics: (1) recognize negative automatic thoughts when patient feels worst, (2) dispute negative thoughts by focusing on contrary evidence, (3) generate different explanation to dispute negative thoughts, (4) avoid rumination (constant churning of negative thoughts in mind) by consciously controlling thoughts, (5) question negative thoughts and beliefs and replace with empowering positive thoughts and beliefs. Does not involve long psychoanalysis—solution oriented. • Organic/physiological causes: preexisting physical condition, diabetes, heart disease, lung disease, rheumatoid arthritis, chronic inflammation, chronic pain, cancer, liver disease, multiple sclerosis, prescription drugs, antihypertensives, antiinflammatories, birth control pills, antihistamines, corticosteroids, tranquilizers and sedatives, premenstrual syndrome, stress or low adrenal function, heavy metals, food allergies, hypothyroidism, hypoglycemia, nutritional deficiencies, sleep disturbances. • Conduct comprehensive clinical evaluation: ascertain nutritional, environmental, social, and psychological factors; rule out organic factors: nutrient deficiency or excess, drugs (prescription, illicit, alcohol, caffeine, nicotine), hypoglycemia, hormonal de-rangement, allergy, environmental factors, microbes; counseling recommended regardless of underlying organic cause. The focus of this text is on thyroid and adrenal hormones. • Thyroid: depression = early manifestation of thyroid disease: subtle decreases in thyroid hormone can be symptomatic. Whether hypothyroidism results from depression-induced hypothalamic-pituitary-thyroid dysfunction or from thyroid hypofunction is uncertain, but it may be a combination. Screen for hypothyroidism, particularly with suggestive symptoms (e.g., fatigue). • Stress and adrenal function: adrenal dysfunction associated with depression can result from stress. Adrenal stress index measures cortisol and DHEA in saliva. Depression signs: elevated morning cortisol and decreased DHEA. Cortisol elevation reflects disturbed hypothalamic-pituitary-adrenal (HPA) axis and is the basis of the dexamethasone suppression test (DST). HPA dysregulation affecting mood = excessive cortisol independent of stress responses, abnormal nocturnal cortisol release, and inadequate suppression by dexamethasone. CNS effects of increased endogenous cortisol = depression, mania, nervousness, insomnia, and schizophrenia (high levels). Glucocorticoid effects on mood are related to induction of tryptophan oxygenase, shunting tryptophan to kynurenine pathway at the expense of serotonin and melatonin synthesis. • Tests of hypothalamic-pituitary function: DST and thyroid stimulation test—determine if mood is caused by hypothalamic dysfunction and categorize psychiatric illness (e.g., severe major affective disorders vs. severe psychotic disorders). DST—little clinical value for screening and no better than urinary free cortisol. Thyroid hormone assays do not detect all cases of hypothyroidism—not an effective screening procedure. Thyroid stimulation test (TRH) is more sensitive, diagnosing subclinical hypothyroidism. TRH test has wide clinical utility because thyroid dysfunction is implicated in many disorders. TRH grading system for hypothyroidism is as follows: — Grade 3 (subclinical hypothyroidism, 4%): patients without classic hypothyroid signs; normal T3RU, T4, and TSH; abnormal TSH response to TRH test — Grade 2 (mild hypothyroidism, 3.6%): mild isolated clinical signs or symptoms; normal T3RU and T4; baseline TSH elevated; abnormal TRH test — Grade 1 (overt hypothyroidism, 1%): classic hypothyroid signs and symptoms; abnormal lab values (reduced T3RU and T4, increased TSH, abnormal TRH response) • Heavy metals (Pb, Hg, Cd, As, Ni, Al), solvents (cleaning materials, formaldehyde, toluene, benzene, etc.), pesticides, herbicides—affinity for nervous tissue; associated symptoms = depression, headache, mental confusion, mental illness, tingling in extremities, abnormal nerve reflexes, other signs of impaired nervous function (Textbook, “Environmental Medicine” and “Metal Toxicity: Assessment of Exposure and Retention”). • Detailed medical history and hair mineral analysis screen for environmental toxins. If hair mineral analysis is inconclusive, a more sensitive test is the 8-hour lead mobilization test—chelating agent EDTA (edetate calcium disodium) —measure lead excreted in urine for 8 hours after injection of EDTA. • Smoking: major factor contributing to premature death. Nicotine stimulates adrenal secretion (cortisol) = feature of depression. Cortisol and stress activate tryptophan oxygenase, reducing tryptophan delivery to the brain. Brain serotonin depends on amount of tryptophan delivered—cortisol reduces levels of serotonin and melatonin. Cortisol downregulates brain serotonin receptors, reducing sensitivity to available serotonin. Smoking induces relative vitamin C deficiency; vitamin C helps detoxify smoke. Low levels of brain vitamin C can cause depression and hysteria. • Alcohol: brain depressant; increases adrenal hormone output; interferes with brain cell processes; disrupts sleep cycles; leads to hypoglycemia and craving for sugar, which aggravates hypoglycemia and mental and emotional problems. • Caffeine: stimulant. Intensity of response varies greatly—people prone to depression or anxiety are sensitive to caffeine. “Caffeinism” = clinical syndrome of nervousness, palpitations, irritability, and recurrent headache. Students with moderate to high coffee intake score higher on depression scale and have lower academic performance than low users. Patients with depression have high caffeine intake (more than 700 mg/day). Caffeine intake is positively correlated with degree of mental illness in patients with psychiatric disorders. Caffeine plus refined sugar is worse than either alone—combination has clinical link to depression. Average American intake: 150-225 mg caffeine q.d. = 1-2 cups coffee. Some people are more sensitive to effects than others, even small amount in decaf. Patients with psychological disorders should avoid caffeine completely. • Exercise: most powerful natural antidepressant. Benefit in heart health may be related as much to improved mood as to cardiovascular fitness. Profound antidepressive effects—decreased anxiety, depression, and malaise plus higher self-esteem and more happiness; increases endorphins, which are directly correlated with mood. Sedentary men are more depressed, perceive greater life stress, have higher cortisol and lower beta-endorphins than joggers. Depression is responsive to exercise, firming up biochemical link between physical activity and depression; improves self-esteem and work behavior; can be as effective as antidepressant drugs and psychotherapy. Best exercises = strength training (weight lifting) or aerobics (walking briskly, jogging, bicycling, basketball, cross-country skiing, swimming, aerobic dance, and racquet sports).
Affective Disorders
DIAGNOSTIC SUMMARY
DEPRESSION
General Considerations
Therapeutic Considerations
Hormonal Factors
Environmental Toxins
Lifestyle Factors
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Affective Disorders
