Actinic Keratosis
David Cassarino, MD, PhD
Key Facts
Terminology
Actinic keratosis (AK)
Solar keratosis
Atypical intraepidermal proliferation of keratinocytes typically confined to basilar portion of epidermis
Clinical Issues
Older adults typically affected
Mostly occur in Caucasians, much less common in other races
Excellent in vast majority of cases, as only approximately 2-3% progress to invasive SCC
Microscopic Pathology
Basilar budding of atypical cells
Cells show nuclear enlargement, hyperchromasia, and prominent nucleoli
Overlying parakeratosis present
Lesional cells usually do not involve follicles (as opposed to Bowen disease)
Histologic subtypes include hypertrophic, atrophic, pigmented, lichenoid, and bowenoid AK
Top Differential Diagnoses
Squamous cell carcinoma (SCC)
Bowen disease (SCC in situ)
Basal cell carcinoma (BCC), superficial-multicentric and basosquamous types
Melanoma in situ (lentigo maligna type)
Discoid lupus erythematosus
Lichen planus (LP) and lichen planus-like keratosis (benign lichenoid keratosis [BLK])
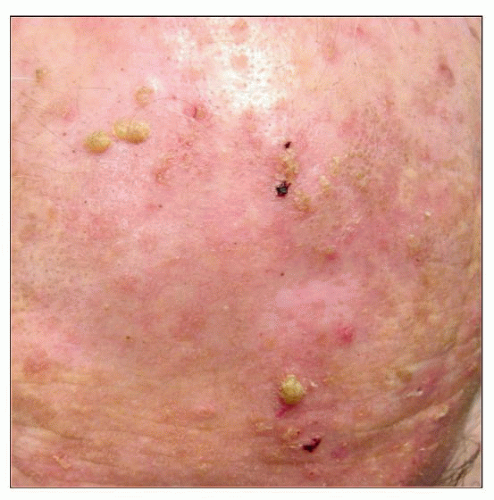 Clinical photograph of the scalp of an elderly patient shows multiple actinic keratoses with prominent crusting. (Courtesy J. Wu, MD.) |
TERMINOLOGY
Abbreviations
Actinic keratosis (AK)
Synonyms
Solar keratosis
Often considered a “precancer” or early squamous cell carcinoma in situ (SCCis)
Definitions
Atypical intraepidermal proliferation of keratinocytes typically confined to basilar portion of epidermis, with very low risk for progression to invasive squamous cell carcinoma (SCC)
ETIOLOGY/PATHOGENESIS
Solar Damage
Ultraviolet light (primarily UVB) induces mutations in DNA, which lead to abnormal proliferation of intraepidermal keratinocytes
P53 mutations are most common genetic alteration identified
CLINICAL ISSUES
Epidemiology
Incidence
Very common lesions, estimated to affect up to 10-40% of adult Caucasians; higher incidence in areas with heavy sun exposure (i.e., Australia)
Age
Older adults typically affected
Gender
Males more common than females
Ethnicity
Mostly occur in Caucasians; much less common in other races
Site
Sun-exposed sites, especially face, head and neck, dorsal hands, and forearms
Presentation
Scaly papules and plaques, often multiple
Natural History
Minority of cases progress to invasive squamous cell carcinoma
Treatment
Options, risks, complications
Controversial whether treatment is necessary in all cases, but most clinicians opt for treatment in order to avoid potential development of SCC
Surgical approaches
Conservative excision of lesions is not necessary in most cases (unless there is clinical suspicion for invasive SCC), but is curative
Drugs
Topical therapy with drugs such as 5-fluorouracil, diclofenac, or imiquimod may be used
Liquid nitrogen (cryotherapy) frequently used
Photodynamic therapy is also an emerging treatment that may be useful for extensive AKs
Prognosis
Excellent in vast majority of cases, as only approximately 2-3% progress to invasive SCC
Most invasive SCCs arising in AKs are low grade, but aggressive cases may also occur
MACROSCOPIC FEATURES
Size
Usually small (< 1 cm) papules, but larger lesions may occur
MICROSCOPIC PATHOLOGY
Histologic Features
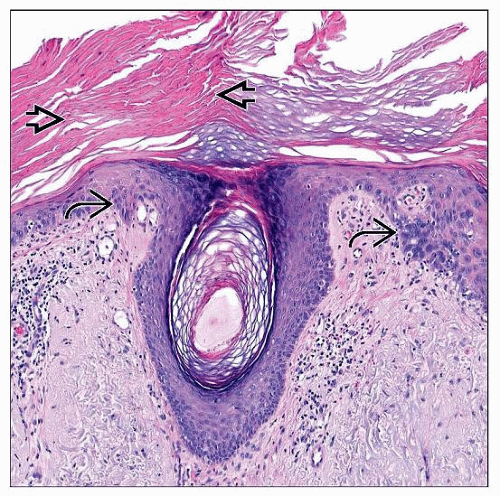
Intraepidermal proliferation of atypical keratinocytes, typically confined to basilar 1/3 of epithelium
Basilar budding of atypical cells
Cells show nuclear enlargement, hyperchromasia, and prominent nucleoli
Abundant eosinophilic-staining cytoplasm
Increased numbers of mitotic figures usually present
Overlying parakeratosis present in vast majority of cases; hypogranulosis may also be present
Lesional cells usually do not involve follicles (as opposed to Bowen disease) and adnexal ducts
Leads to alternating “red and blue” tiers of parakeratosis (overlying AK) and hyperorthokeratosis (overlying follicles and eccrine ducts)
Histologic subtypes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree