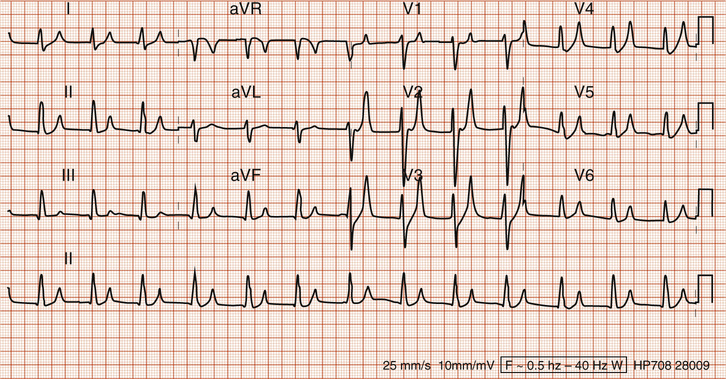
Daniel Martinez A thorough history and physical exam is the cornerstone of effective medical treatment. However, it is not always appropriate to delay workup and treatment until a formal history and physical exam has been completed. This is often the case in the emergency room setting where the top priority is to rule out life-threatening conditions. In the appropriate clinical setting (such as a middle-aged male with diabetes), a patient who presents with cardiac symptoms such as palpitations or chest pain should be evaluated with a STAT electrocardiogram (ECG), serial cardiac enzymes (i.e., troponin levels), and basic labs such as a basic metabolic panel and complete blood count. The ECG shows a regular pulse rate (around 70 beats/minute), regular rhythm, and normal axis. However, the P waves are difficult to appreciate. This makes it difficult to interpret whether the patient is in normal sinus rhythm or not. There is a widened QRS complex (greater than three small boxes) and peaked T waves. The Q-T intervals are normal (less than half the distance between the R-R intervals). There are no ST segment changes, Q waves, or T wave inversions to suggest new or old cardiac ischemia. The most clinically relevant aspect of this ECG is the widened QRS complex. It indicates that there is an abnormal slowing of the electrical conduction through the heart during systole. This can be seen in a bundle branch block, ventricular paced rhythm (because the bundle of His is bypassed), or electrolyte abnormality causing action potential slowing. There are no findings of a bundle branch block in this ECG, so that is less likely. The absence of P waves initially suggests a ventricular-paced rhythm. However, the normal QRS axis and upright T waves throughout the ECG point against this. Taken together, these findings more likely suggest a severe electrolyte abnormality. However, an ECG interpretation should always be done with consideration of the clinical picture as a whole. Potassium is a key component of the action potentials that propagate the electrochemical signal throughout the heart. Thus, changes in its serum concentration can dramatically affect an ECG. Most medical students and residents remember the peaked T waves seen in hyperkalemia; however, this is not the most important change seen because it is generally associated with moderate levels of hyperkalemia. More important to remember are the ECG changes found as hyperkalemia worsens to dangerously high levels. At this point, an ECG can show a widened QRS complex, prolonged PR interval, absence of P waves, and finally a sine wave ECG morphology. Because these ECG findings are seen at more extreme levels of hyperkalemia, they are the most clinically important to remember. Patients with mild hyperkalemia are often asymptomatic. However, as hyperkalemia worsens, patients can present with nonspecific symptoms of fatigue, weakness, nausea, and abdominal pain. They can also have more severe symptoms such as paresthesias, muscle weakness/paralysis, and cardiac palpitations. Untreated hyperkalemia is extremely dangerous because of its pronounced effects on cardiac electrophysiology. It affects the resting membrane potential, action potential velocity/duration, and electrical propagation through the heart. The first step in the emergent treatment of hyperkalemia is to stabilize the cardiac membrane by mitigating the adverse electrophysiologic effects of potassium. This is done by giving intravenous (IV) calcium. Calcium gluconate 10 mL of 100 mg/mL given intravenously over 2 to 3 minutes is a typical dose. (Calcium chloride also can be used but generally at lower doses.) This treatment helps to reverse the ECG changes described above but works only for about 30 to 60 minutes. Thus, it is also important to lower potassium levels shortly after membrane stabilization. Also, it is important to remember that IV calcium is relatively contraindicated as a treatment for hyperkalemia that is caused by digoxin toxicity. Digoxin toxicity is a unique scenario. Although hyperkalemia is often seen because the Na-K adenosine triphosphatase (ATPase) enzyme is impaired by digoxin, the hyperkalemia itself is generally not what would kill the patient. Primary treatment of the hyperkalemia itself is not the first step to take. Instead, fragment antigen-binding (Fab) fragments (antibodies against digoxin) should be administered promptly when digoxin toxicity is diagnosed. This also helps correct the hyperkalemia because the Na-K ATPase enzymes begin to work again (see Fig. 58.2).
A 55-Year-Old Male With Diabetes on an Angiotensin-Converting Enzyme (ACE) Inhibitor
How do you manage these symptoms in the emergency room setting?
How do you read the patient’s ECG?
What are the ECG changes found in hyperkalemia?
What are the clinical manifestations of hyperkalemia?
How do you emergently treat hyperkalemia?
58 A 55-Year-Old Male With Diabetes on an Angiotensin-Converting Enzyme (ACE) Inhibitor
Case 58