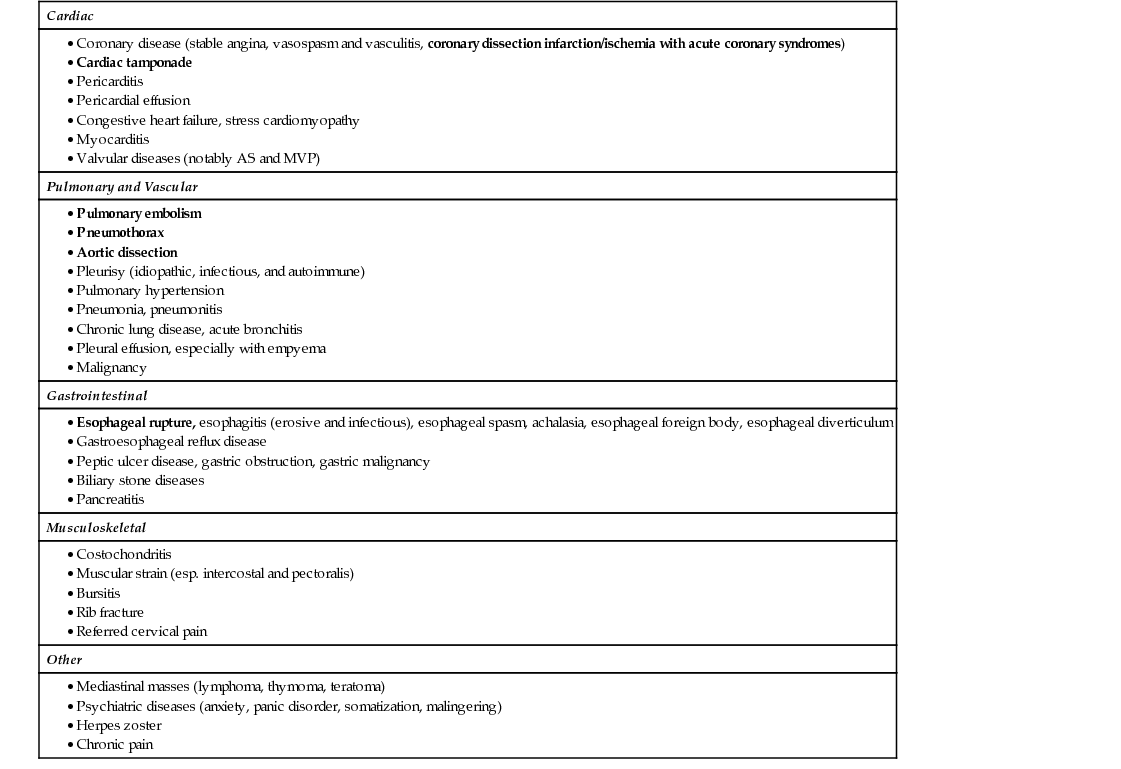
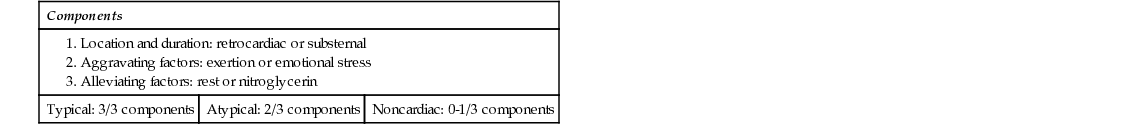
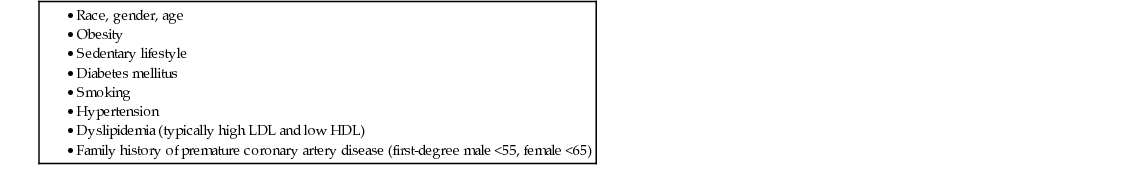
Seth Politano A broad differential diagnosis should be undertaken with a chief complaint of chest pain (see Table 55.1). Particular attention should always be focused first toward life-threatening causes of chest pain, then other serious (but not immediately life-threatening) causes, then finally less ominous causes. With some of the life-threatening causes of chest pain, it is important to note that “pain” might not be the patient’s chief complaint. Patients often describe a stabbing, crushing, pressurelike, or tearing sensation. Therefore, sometimes using alternate words to ask a history, including “chest discomfort,” may be useful. Asking the patient if he or she has current chest pain is helpful for triage. Always obtain the usual elements, including prior events, onset/timing, location, severity, intensity, and alleviating and aggravating factors, as well as baseline functional status and exercise capability/limitations. It is important to undertake a complete medication history, family history, and social history and to elicit historical evidence of features that are characteristic for life-threatening causes of chest pain. Table 55.2 lists historical features of life-threatening causes of chest pain. TABLE 55.2 Historical Features of Life-Threatening Causes of Chest Pain After asking the patient salient features of conditions that are life-threatening, one can then investigate other causes of chest pain. A general review of systems will oftentimes elicit the relevant symptoms seen in these disorders. Specific questions to ask include those related to fever, weight loss, cough, edema, abdominal pain, food association, joint pain, rash, weakness in extremities, and psychiatric screening. Table 55.3 lists physical exam findings with select causes of chest pain. TABLE 55.3 Physical Exam Findings With Select Causes of Chest Pain The definition of angina is chest pain or discomfort that may be pressurelike, a sensation of fullness or squeezing; it can be felt in the chest, jaw, shoulder, back, or arm. The pain is usually less than 5 minutes in duration. In a patient presenting with chest pain, and when angina is suspected, it is useful to classify the chest pain into anginal categories depending on historical information (see Table 55.4). Table 55.5 lists the risk factors for underlying CAD. The pretest probability for underlying CAD is useful for risk stratification in the outpatient setting and can guide the need for noninvasive testing. It also provides you with a tool to consider if CAD is the likely cause of the patient’s presentation with chest pain. Table 55.6 lists estimated risks for CAD. TABLE 55.6 Estimated Risk of Coronary Artery Disease
A 58-Year-Old Male With Chest Pain
What do you consider in your differential diagnosis of the chest pain in this patient?
What other historical elements can you use to elicit the history in a patient with chest pain?
Condition
Clinical Hints/Findings
Myocardial Infarction/Ischemia
Prior history, risk factors, location in the retrosternal/left side, worse with exertion, alleviated with rest or nitroglycerin.
Aortic Dissection
Severe tearing pain radiating to back. May also present with strokelike symptoms (i.e., weakness in lower extremities). Can also present with symptoms from complications, including pleural effusion and ischemia.
Pneumothorax
Sudden dyspnea and chest pain that is pleuritic in nature.
Cardiac Tamponade
Shortness of breath, weight loss (in a patient with malignancy-associated tamponade), fevers (in a patient with infectious or autoimmune disease-associated tamponade)
Pulmonary Embolism
Sudden dyspnea and chest pain that is pleuritic in nature. May have nonproductive or productive cough with hemoptysis. Risk factors include immobility, malignancy, smoking, oral contraceptive pills (OCPs), and inherited thrombophilias.
Esophageal Rupture
Sudden tearing pain. Recent straining, coughing, ingestion of caustic substances. History of reflux, carcinoma. Patients may also have back pain, referred shoulder pain, or abdominal pain.
What physical exam clues can you use with a chief complaint of chest pain?
Condition
Clinical Hints/Findings
Myocardial Infarction/Ischemia
May have S3 (as seen in patients with acute heart failure) or S4 (as seen in patients with underlying coronary artery disease or hypertension) on exam. Murmur from onset of valvular disease or wall rupture. May also present with signs of low-output (hypotension, altered mental status) or volume overload (crackles, jugular venous distention, edema).
Aortic Dissection
Blood pressure difference in arms, murmur of aortic insufficiency, objective weakness in lower extremities, decreased pulses in lower extremities. Complications include hypotension, and exam findings consistent with pleural effusion and ischemia.
Pneumothorax
Decreased breath sounds, hyperresonance to percussion. Can see tracheal deviation with tension pneumothorax.
Cardiac Tamponade
Jugular distention, decreased breath sounds, hypotension, pulsus paradoxus.
Pulmonary Embolism
Tachycardia, tachypnea, hypoxia. Can have signs of deep vein thrombosis (DVT) and pleural effusion. Loud P2, fixed split S2.
Esophageal Rupture
Tachycardia, palpable subcutaneous emphysema, Hamman’s sign (audible crunch with heart sounds).
Pulmonary Hypertension
Loud P2, fixed split S2, heave, eventual right-sided heart failure (jugular venous distention, pulsatile liver, edema).
Congestive Heart Failure
Jugular venous distention, hepatojugular reflux, S3, S4, crackles, exam evidence of pleural effusion, may hear wheezing, pulsatile liver/hepatomegaly/ascites, dependent edema, pulsus alternans.
Pericarditis
Friction rub. May be tachycardic and febrile. Lymph node, joint exam, and skin exam may reflect causes (i.e., autoimmune diseases, infection, malignancy, uremia). Kussmaul’s sign (increased jugular venous distention or lack of decrease with inspiration) if constrictive.
Pneumonia
Fever, bronchial breath sounds, rhonchi, dullness to percussion, friction rub, signs of effusion.
Aortic Stenosis
Lack of normal carotid upstroke, systolic crescendo–decrescendo murmur which is loudest at the right upper sternal border that radiates to supraclavicular/carotid region. S4 may be present, and heart sounds may be paradoxically split or reveal the absence of A2 heart sounds.
Does this patient have angina?
What are the risk factors for coronary artery disease?
Given historical components, what is this patient’s pretest probability of underlying coronary artery disease?
Typical Angina
Atypical Angina
Nonanginal
Male
Female
Male
Female
Male
Female
30-39 Years
59
27
29
10
18
5
40-49 Years
69
37
38
14
25
8
50-59 Years
77
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

55 A 58-Year-Old Male With Chest Pain
Case 55