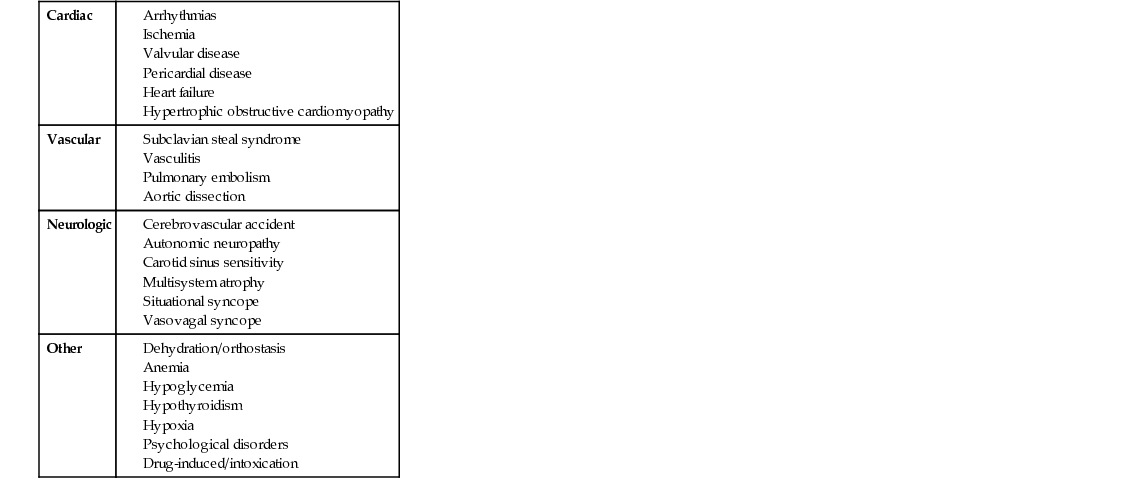
Patrick E. Sarte, Seth Politano, Eric Hsieh In a patient presenting with syncope, one can divide up the etiology into broad categories, of which the majority are cardiac and neurologic in origin. However, as can be seen in Table 48.1, other causes include pulmonary, vascular, and even psychiatric. The presence of a murmur on cardiac exam suggests a cardiac etiology, particularly a valvular disorder. In addition to the patient’s age, the description and location of the murmur are most consistent with aortic stenosis. A definitive diagnosis is established with echocardiogram. Aortic stenosis classically has a systolic ejection murmur with a crescendo–decrescendo quality heard best in the aortic area (i.e., the right second intercostal space) with radiation to the carotids. When severe, there is a characteristic delay and decrease in the intensity of the pulse, which is also referred to as pulsus tardus et parvus. Patients may also have an audible S4 and laterally displaced point of maximal cardiac impulse because they develop concentric left ventricular hypertrophy as a compensatory response by the left ventricle to pump blood across a stenotic aortic valve to maintain systemic perfusion pressures. The patient may likewise have the same physical findings of congestive heart failure such as elevated jugular venous distension, bibasilar rales on pulmonary auscultation, and/or lower extremity pitting edema in advanced cases of aortic stenosis. The typical maneuvers that are performed and that affect the murmurs of valvular disorders are the Valsalva maneuver, passive leg raise, and hand grip (Table 48.2). The Valsalva maneuver is performed by asking the patient to bear down, which causes an increase in intrathoracic pressure and thus a decrease in venous return. The passive leg raise is performed by the examiner on the patient in the supine position, and this results in an increase in venous return. The hand grip is performed by the patient, and this causes an increase in afterload. During a Valsalva maneuver, as the venous return decreases, the gradient across the stenotic aortic valve also decreases, and thus the magnitude of the murmur decreases as well. The opposite effect on the aortic stenosis murmur is achieved when a passive leg raise is performed, which increases the venous return to the heart and increases the pressure gradient across the stenotic aortic valve. Finally, as mentioned above, the hand grip leads to an increase in afterload, which causes a decrease in the pressure gradient across the stenosed aortic valve, and this results in a diminishment of murmur intensity.
A 67-Year-Old Male With Syncope
What are the considerations for the differential diagnosis of this patient’s presenting symptom?
Given this physical exam, what do you think is the most likely cause of this patient’s syncope?
What are the physical exam findings of aortic stenosis?
What maneuvers are performed to accentuate or diminish the murmur associated with aortic stenosis, and why do they have that effect?
48 A 67-Year-Old Male With Syncope
Case 48