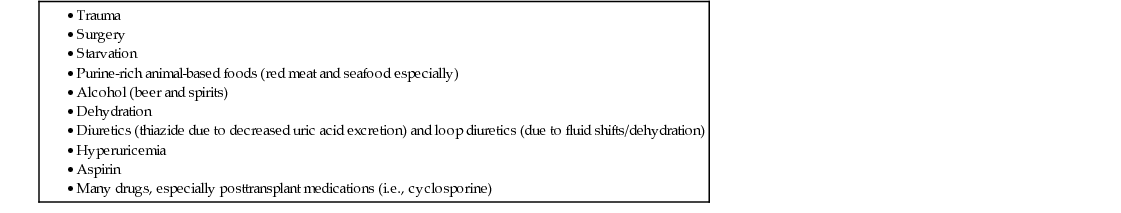
Dawn Piarulli, R. Michelle Koolaee This is a patient presenting with an acute polyarticular inflammatory arthritis. The causes of polyarticular arthritis include but are not limited to: • Other infections (i.e., tubercular and fungal organisms, Borrelia burgdorferi [Lyme disease]) • Crystal-induced arthritis (i.e., gout, pseudogout, calcium oxalate, hydroxyapatite) • Endocrinopathies (i.e., hyperparathyroidism, hyperthyroidism, hypothyroidism) The acuity of his symptoms makes causes such as crystal-induced arthritis very likely (especially gout, given his comorbidities, along with use of diuretics; calcium oxalate crystals is less common but is seen exclusively in patients with CKD). An infectious arthritis is also possible, given the acuity of the symptom. A systemic rheumatic illness is unlikely; these tend to present with chronic inflammatory arthritis. This patient has multiple nodules of the extensor surfaces of his joints. The differential diagnosis of nodules includes xanthoma (history of hyperlipidemia), rheumatoid nodules (multiple joints involved), sarcoidosis (usually located on the lower rather than upper extremities), tumors (less likely to be present in multiple locations superficially), and tophi (which are due to deposition of monosodium urate crystals in and about the joints of a gout patient). Given the location of the nodules, along with the acuity of his arthritic symptoms, his nodules likely represent tophi (nodules in RA and sarcoidosis would be associated with a chronic inflammatory arthritis). Figure 47.1 represents examples of gouty tophi. Furthermore, based on his comorbidities (obesity, type 2 diabetes, CKD, and hypertension; all of which are associated with gout), likely tophi in the elbows, and the onset of symptoms during hospitalization for diuretic therapy, the most likely diagnosis is acute polyarticular gout. Table 47.1 highlights the common risk factors for gout flares. The best way to determine the etiology of any arthritis with effusion is arthrocentesis. Synovial fluid analysis is a valuable tool to help in the diagnostic workup. The leukocyte count above 2,000/mm3 confirms the presence of inflammatory fluid. Figure 47.2 demonstrates monosodium urate (MSU) crystals, which have the characteristic needle-shaped appearance and are negatively birefringent on polarized light microscopy; this is the definitive way to diagnose gout. Septic arthritis can rarely occur simultaneously as an acute gout flare, but the leukocyte count is usually over 50,000/mm3. Table 47.2 compares synovial fluid findings in patients with inflammatory versus noninflammatory arthritis.
A 63-Year-Old Male With Acute Polyarticular Arthritis
What is the differential diagnosis for this patient’s joint pain?
How does the physical exam in this case help to narrow the differential diagnosis?
What is the single best test to help determine the diagnosis?
How do you interpret the synovial fluid analysis results?
47 A 63-Year-Old Male With Acute Polyarticular Arthritis
Case 47