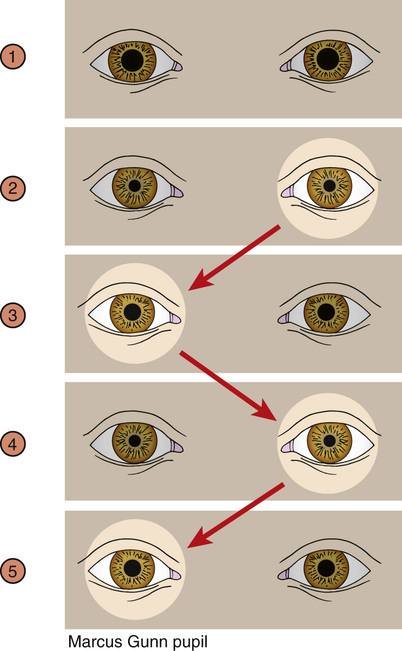
Albert Huang, John Khoury A potential cause of hand numbness is peripheral nerve entrapments involving the radial, ulnar, or more commonly the median nerve within the carpal tunnel, also referred to as carpal tunnel syndrome (CTS). It is important to inquire about work or recreational activities that result in repetitive actions. In today’s technological society, heavy use of mobile devices or poor ergonomic wrist placement while typing can result in hand numbness due to CTS. Other activities that result in median nerve damage include frequent wrist flexion while operating machinery or regularly using tools such as wrenches, screwdrivers, and even surgical instruments. Examples of occupations that can lead to repetitive wrist or hand motions include secretaries, mechanics, and surgeons. Other common causes for upper extremity paresthesias include cervical spine pathology, such as a disc herniation or arthritic facet joint spaces leading to narrowed neuroforamen and ultimately damaged nerves exiting the cervical spine. Chronic conditions can result in damage of smaller nerves fibers distally and raise the question of hypothyroidism or diabetes mellitus. However, in this particular case, cervical spine pathology would more commonly present unilaterally and a metabolic cause is less likely considering the patient’s younger age (see Table 38.1). The swinging light test is commonly utilized to assess both afferent and efferent function of the optic nerves. This test is conducted by swinging a pen light from one eye to the other and assessing for symmetrical bilateral pupil dilation. Despite light being shown in only one eye, the normal response is bilateral pupil constriction. When there is unequal pupil constriction, the examiner must determine whether the cause is due to an afferent or efferent defect. If there is an afferent defect, both pupils demonstrate a symmetrical decreased constriction of the pupils when the light is shone in the affected eye. If the defect is efferent, only the affected eye demonstrates an unequal and diminished pupillary constriction when compared to the unaffected eye no matter which side the light is shone. An afferent pupillary defect is also known as a Marcus Gunn pupil and is commonly seen in cases of optic neuritis (see Fig. 38.1).
A 32-Year-Old Female With Bilateral Hand Numbness
How can occupational history contribute to the evaluation in this case?
What additional questions are important to ask related to the numbness and tingling in her hands?
How is optic neuritis commonly tested on physical exam?
What is the importance of this electrical sensation running down the back?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


38 A 32-Year-Old Female With Bilateral Hand Numbness
Case 38