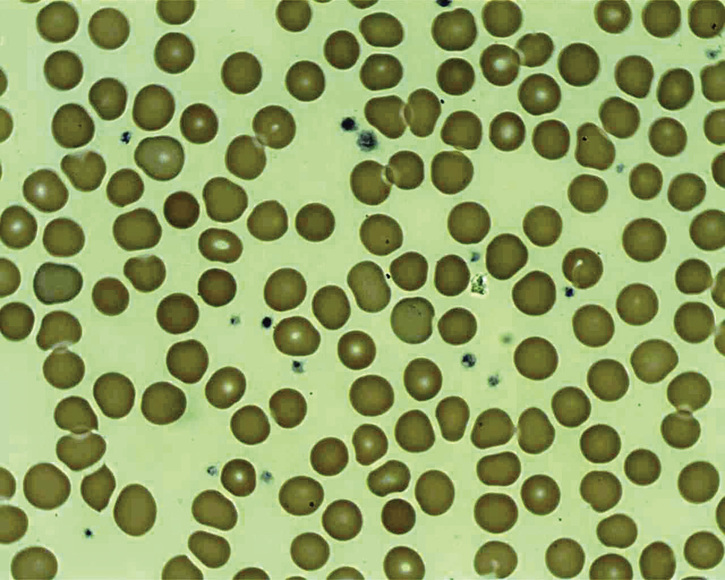
Monisha Bhanote, Daniel Martinez Pregnancy should be considered in any female of reproductive age with nonspecific symptoms such as fatigue. Taking a sexual history and ordering a pregnancy test is therefore important in the evaluation. Hypothyroidism is also a reasonable consideration, and a screening thyroid stimulating hormone (TSH) is generally indicated. Many rheumatologic diseases can cause fatigue, and thus a thorough review of systems and a physical exam that includes the skin, joints, and nails are also important; these will help narrow down which of the many rheumatologic tests are indicated if at all. Anemia can cause fatigue in all populations, and a complete blood count (CBC) is generally ordered. Macrocytosis refers to the presence of abnormally large red blood cells. This can be associated without anemia as in cases of newborns or during pregnancy. It can also be associated with anemia due to many other causes (see Table 37.1). Many of the pathologies listed have other significant clinical or laboratory abnormalities that would make the diagnosis easy to make (such as liver disease or an acute leukemia). However, in a patient with macrocytosis who has an otherwise normal clinical exam and labs, the main differential is between vitamin B12 and folate deficiency. The workup includes a peripheral smear, checking a reticulocyte count to confirm the anemia is due to decreased production, and ordering B12/folate levels. If B12 and folate levels are normal and there remains a high suspicion for deficiency, then homocysteine and methylmalonic acid levels can be ordered as they are more sensitive. Vitamin B12 deficiency can be seen in decreased intake, poor absorption, and increased need. Therefore, vitamin B12 deficiency can happen in individuals who are vegan as well as vegetarians who do not consume enough milk, eggs, or cheese and do not supplement the vitamin in other ways. However, the average person’s vitamin B12 stores can lasts several years without any signs or symptoms of deficiency. This makes it difficult for decreased vitamin intake to be the sole reason for the significant deficiency seen in this patient. A good clinician would consider other reasons for a vitamin B12 deficiency in a young person who has only been a vegan for a couple years. Vitamin B12 deficiency can also be seen in certain medical conditions such as atrophic gastritis, Crohn’s disease, celiac disease, bacterial overgrowth, parasitic infections, immune disorders (Grave’s disease or lupus), and weight loss surgery, which can cause loss of part of the gastrointestinal tract that absorbs nutrients. Malabsorption is characterized by abnormal or suboptimal absorption of nutrients (fats, vitamins, proteins, carbohydrates, electrolytes, and minerals) across the gastrointestinal tract. It can include one or multiple nutrients depending on the abnormality. Malabsorption can be subclassified into three categories: selective, partial, and total. Selective malabsorption is seen with specific nutrients such as lactose intolerance. The causes of malabsorption can be due to infective agents, structural defects, surgical changes, mucosal abnormalities, enzyme deficiencies, digestive failure, and systemic diseases (see Table 37.2).
A 20-Year-Old Female With Chronic Fatigue
What should be reasonably considered in a young female with new fatigue?
What are the pathologic causes of macrocytic anemia and how do you work it up?
What etiologies should be considered for a patient with vitamin B12 deficiency?
What are common causes of malabsorption syndromes?
37 A 20-Year-Old Female With Chronic Fatigue
Case 37